SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.
 Anyone reading the news cannot be faulted for being alarmed by the grisly HIV-AIDS situation in the country.
Anyone reading the news cannot be faulted for being alarmed by the grisly HIV-AIDS situation in the country.
For one thing, the number of HIV-AIDS cases reported has been rising at an exponential rate since 1984. Figure 1 below — using latest data from the HIV and AIDS Registry of the National Epidemiology Center of the Department of Health (NEC-DOH) — shows how the number of cases has risen from an average of 83 cases a year during the ’80s and ’90s to an average of nearly 800 cases a year since 2000.
There’s also no hint of the trend slowing down: just last May 2013, the number of new HIV cases per month reached a record high of 415 cases. This contributes to the alarming fact that there has been a whopping 1,490% increase in the number of recorded cases from 2005 to 2012. Also, a mind-blowing 74% of the total reported cases since 1984 came in just the past 5 years.
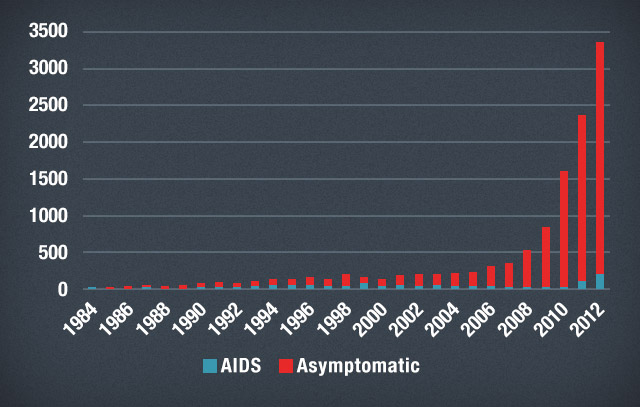
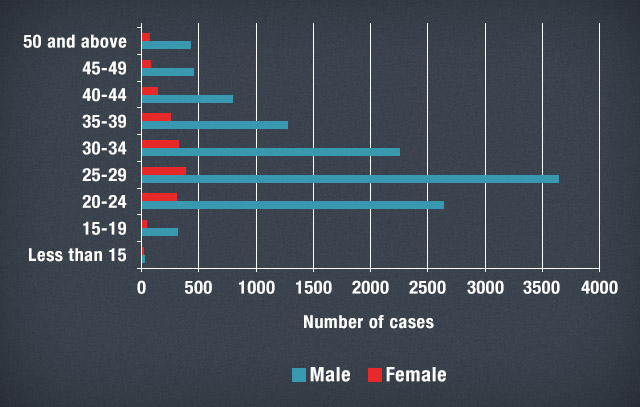
Figure 2 below shows that a disproportionate number of reported HIV-AIDS cases in the country involves males (87.6%). A considerable 72% of them fall under the 20-34 age bracket, while almost a third (31%) of them fall under the narrower 25-29 age bracket.
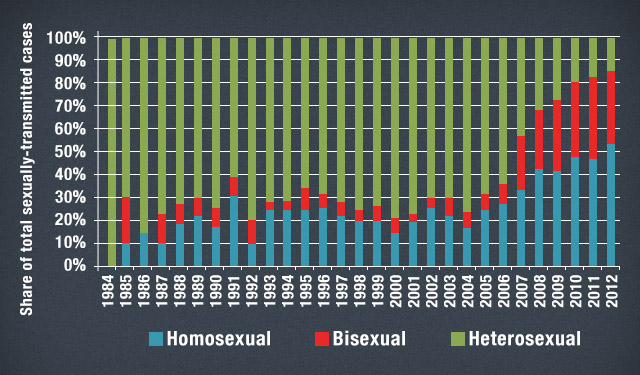
A great majority of the known cases of HIV from 1984 were reportedly transmitted through sexual contact (94%). However, there has since been an emergent trend of homosexual and bisexual transmission taking on a larger proportion of total sexually-transmitted cases in recent years, as shown in Figure 3 below.
Whereas heterosexual transmission constituted nearly three-quarters (74%) of annual cases on average from 1984 to 2006, its share has since considerably declined to around a quarter (26%) of annual cases on average since 2007.
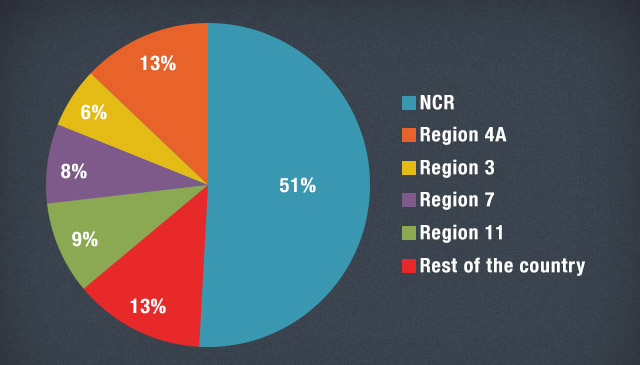
HIV also seems to be largely an urban phenomenon, at least according to addresses indicated in reported cases at the time of diagnosis (Figure 4 below). According to total data from January 1984 to May 2013, about half (51%) of the total reported cases came from NCR, followed by nearby Calabarzon (13%), Central Luzon (9%), and then Central Visayas (8%) and Davao Region (6%).
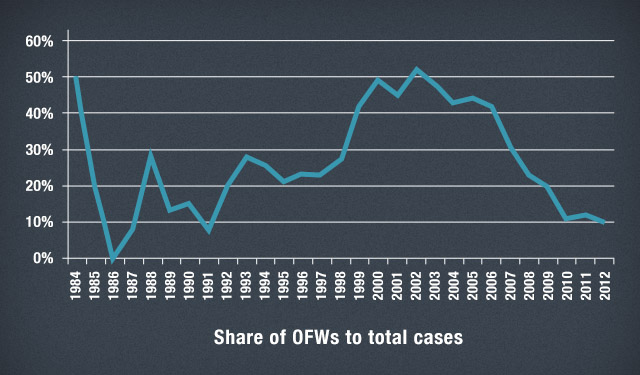
Finally, OFWs constitute around 17% of total reported HIV cases since 1984. Most cases were males (80%) with sexual contact being the predominant mode of transmission (94%), mostly through heterosexual sex. The data show that OFWs constituted a steadily increasing proportion of total cases throughout the ’90s, but the trend has since declined in the past decade (as shown in Figure 5 below). This coincides with a precipitous increase in the number of cases accounted for by non-OFWs in recent years.
In summary, the grim statistics seem to suggest a worsening HIV epidemic in the country, affecting on average (and especially in recent years) non-OFW males aged 20-34 situated in or near urban regions and engaged in non-heterosexual sex.
That a worsening HIV epidemic is already upon us has, in fact, already been acknowledged by DOH officials in Cebu City, some public health experts, and no less than Health Secretary Enrique Ona.
Indeed, the Philippines seems to be defying the global decline in the annual number of new HIV infections, according to the 2012 UNAIDS Report on the Global AIDS Epidemic. Whereas 39 countries (many of which come from Sub-Saharan Africa) have seen declines in the incidence of HIV among adults by more than 25% since 2001, the Philippines is among the 9 countries in the world that have seen steep increases in the number of newly infected people by at least 25% compared to 2001 incidence rates.
Our failure to reverse the spread of HIV-AIDS in the country also reflects on our imminent failure to fulfill Goal 6 of the Millennium Development Goals. It is one of 3 main areas which contribute to the low probability of the country attaining targets by 2015.
Prevention vs cure
Such a gargantuan public health problem seems, at the outset, too large to combat. But despite the mammoth task facing everyone (not just government), there are useful starting points for identifying solutions.
For one, some studies point out that, at least from an economic point of view, preventing HIV is indeed better than curing it. This is especially relevant to developing countries like the Philippines where resources to combat HIV-AIDS are severely constrained.
Research shows that among the most cost-effective measures are mass media campaigns (whether through television, radio, newspapers, or the Internet) that disseminate information and help educate the general public. This is followed by peer education among sex workers, condom distribution, and voluntary procedures that involve diagnosis, counseling, and testing.
Anti-retroviral therapy, on the other hand, is listed among the least cost-effective measures to combat HIV-AIDS. It’s at least 80 times more costly than mass media campaigns, which are considered among the cheapest buys. Estimates also suggest that, at least in Africa, anti-retroviral therapy could reduce the number of new infections by only 40,000 yearly, while preventive measures can avert as much as 3.53 million new infections yearly.
To some extent the DOH already realizes the advantages of HIV prevention over cure. However, the agency is hard-pressed to pursue massive prevention campaigns due to very tight budget constraints.
Assistant Secretary Eric Tayag has indicated that the government needs at least P35 billion to fund its HIV prevention programs from 2011 to 2016. Yet the DOH has secured only P19 billion from local and foreign sources. Where it will get the remaining P16 billion remains a puzzle that our legislators could potentially (and will hopefully) address in the upcoming 16th Congress.
A case for the RH Law
As a final point, since the HIV-AIDS epidemic is largely borne by unprotected sex, it is imperative that safe sex be promoted as much as possible. Condoms, when properly and consistently used, are considered an integral part of the global campaign of HIV prevention. That is why it is preferable to break down all barriers which prevent their use — especially among the sexually active segment of the population.
The RH Law could help in this regard. By providing the mandate to local government units to provide for contraceptives such as condoms, the RH Law can play a key role not only in the reproductive health front, but also in the HIV-AIDS prevention front.
However, the recent debacle regarding the TRO slapped against the law, and the consequent halt in its implementation, sends the wrong signals about the government’s commitment to stop the spread of HIV-AIDS. It gives the impression that there still exist considerable social stigmas around the free use of condoms across the board — whether they are used for reproductive health or not.
While the merits of the RH Law are being debated, hundreds (if not thousands) of lives are at risk because access to contraceptives like condoms is not as free as it should already be. One can only hope that the ensuing oral arguments proceed as quickly as possible and result in a decision favorable to the full and unhindered implementation of the RH Law. As a result, every packet of condom will go a long way in preventing the further spread of HIV, one sexual encounter at a time.
Stigma as a critical constraint
Preventing the spread of HIV need not be too complicated or too costly. As studies have shown, measures as straightforward as information campaigns and condom distribution can go a long way in averting the number of new HIV cases in a more cost-effective manner. We already even have a law which could potentially address these concerns at the same time, and address the attendant budget constraints.
What’s really preventing us from fully addressing the problem, therefore, are not the technical or financial constraints but the institutional constraints, consisting of both formal rules (e.g., the TRO against the RH Law) and informal norms (i.e., the continuing stigma against condom use and discrimination against people afflicted with HIV).
Battling HIV requires a buildup of positive attitude and self-confidence among the people who are afflicted or potentially afflicted. Stigmas and discrimination regarding sex, condom use, and HIV-AIDS only serve to compound (and not lessen) the burden felt by these people. To my mind, only when we finally break down these misconceptions and biases will the fight against HIV-AIDS truly take flight. – Rappler.com
The author is a summa cum laude graduate of the UP School of Economics. His views are independent of the views of his affiliations.
Add a comment
How does this make you feel?
There are no comments yet. Add your comment to start the conversation.