SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.

This compilation was migrated from our archives
Visit the archived version to read the full article.
ILOILO CITY, Philippines – It all started with a simple Facebook message.
“Hi, how are you? Where are you from?” began the conversation.
Jake*, 21, responded to the message, and started a flurry of exchanges with his new friend online. It went on for weeks – getting to know each other, sharing personal information, and later, talking about sex.
His 24-year-old online friend did not have any photos on his profile, but he did send Jake a photo of himself. “I never expected him to be so good looking, with a nice body,” Jake said.
They met in person weeks later.
It was only Jake’s second time to have sex ever. The first time had been when he was just 18, with a friend, but this one was the first time he had ever slept with someone he met online.
They had sex that one time, and never again. But once was enough to change the rest of Jake’s life.
First, his weight dropped so rapidly, his cheeks became sunken, his face more gaunt. Then his throat started to hurt, became sore and painful, making it harder to swallow. In the evening, he woke up in cold sweats, sheets soaked, despite air conditioning on full blast.
And then the flu-like symptoms went away in a week, as quickly as they came. “Just a fever,” he thought.
Jake graduated a few months later, among the top of his class, with cum laude honors. He was all set to become a seafarer, and was scheduled to embark on a ship for his first job.
But Jake never made it onboard. The symptoms were a sign of something much more serious than the flu.
Jake was HIV positive.
When it hits
“I was actually crying not because I was positive. I was crying because I was thinking I won’t be able to fulfill my dreams for my family,” he said, remembering the moment he found out. “Because you know the discrimination, the stigma, the restrictions in terms of working environment, especially at sea.”
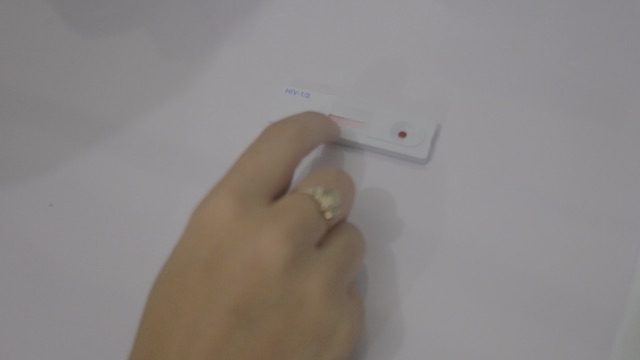
Jake had taken the human immunodeficiency virus (HIV) test on a complete whim, after HIV educators came to campus to inform students about its risks, bringing testing gear with them.
He took the test without fear or worry – “I am not that aggressive in terms of sex, it was only my second time” – but did so out of convenience. There was no doubt in his mind about his status, even when his friend got a sealed envelope and he got nothing. Not even when he was made to wait for two hours. Or when he was called to come inside, unlike those who came before him.
And then the news came – a sudden hit, like a bolt of lighting, unexpected, but with such precision and intensity. There was no question of “Are you sure?” or “It can’t be true,” but only a shock that very quickly gave way to knowing how the virus came to be in him.
“When they told me that I was positive, I just cried. Then I asked them, ‘What’s next?’ I didn’t know what to do. Like after graduation, ‘What’s next?’ I just didn’t know what to do after that.”
Before the diagnosis, Jake had never learned about HIV, never used a condom or learned about how to properly use one, never knew there was a risk of being infected. Neither did he know that he, a sexually active millennial, was highly susceptible to contracting the virus.
Jake’s case is common in a disturbing way: he is part of the age group that is seeing the largest increase in HIV infections.
It’s an old virus, but with new victims. Young, sexually active millennials are seeing a rise in HIV infections across the world, a trend that does not spare the Philippines.
Out of the 42,283 HIV-positive recorded individuals in the country as of March 2017, 11,550 are from the 15-24 age group in the country, according to a Department of Health (DOH) report. That’s 8th graders, high schoolers, and college students.
Social media
And how does this age group get infected?
Sex, of course. Made infinitely easier by social media.
With technology so readily available, finding sexual partners is as easy as a swipe to the right, clicking a follow button, or sending suggestive pictures and messages to strangers.
“They use Grindr, Facebook, or Twitter, to meet other guys for these risky behaviors,” said Robert Figuracion Jr, an HIV coordinator in Iloilo City, referring to dating and social media apps.
Jake said that while he doesn’t personally have Grindr or Tinder, he often receives messages from random strangers on Facebook: “Hi, are you straight?” “Top or bottom?” “Want to meet up?” Even older men send messages, he said, men looking for sex with younger, less experienced millennials.
“That’s really how the current generation does it – through chat. They befriend you. Then when things seem to be going well, they ask you to send naked photos.”
And then, there’s something else that technology and Facebook help organize easier.
“These happen really pretty often. Like every month,” Figuracion said. “There are also ‘group activities’ or orgies.”
The orgies, coordinated online and largely through Facebook, attract not just men who have sex with men, but bisexuals, and sometimes straight couples too.
In addition to technology, lines are often blurred when it comes to sexuality, which has become more fluid. Individuals have sex with both males and females but don’t consider themselves gay; transgender women have sex with males; teenage girls have sex with males who have been with other males.
Even those who are faithful to their partners may contract HIV, if their partners secretly have sex with other people, or if they are in open relationships.
Jake for instance, is gay, while his former partner identified as a bisexual.
Of the 15-24 infected individuals in the Philippines, the DOH report said, 96% were infected through sexual contact – 6,196 said they engaged in homosexual sex, 1,357 in heterosexual sex, and 3,500 in bisexual sex.
Focus on the youth
While the age group with the highest number of HIV positive individuals remains to be 25-34 (51.3%), the proportion of HIV-positive cases in the 15-24 year age group increased from 25% in 2006-2010, to 29% in 2011-2017, according to DOH data.
This is why HIV advocates in the country have shifted their resources and focus to the youth.
‘They use Grindr, Facebook, or Twitter, to meet other guys for these risky behaviors.’
– Robert Figuracion Jr, HIV coordinator in Iloilo City
“The sadder part is young people are still dying. We see that week after week,” Figuracion, who works at the Family Planning Organization of the Philippines (FPOP) office in Iloilo City, said.
“Just this week here at FPOP, we diagnosed 4 in 4 days. 3 of them are 15-24. Only one was a 43-year-old and two of the 15-24 are already manifesting opportunistic infections – pneumonia and tuberculosis,” he said.
“It only means that probably these young people got the infection earlier. Probably as early as 13, 14, when they were back in high school. “
Because many young people are not aware of HIV, they don’t get tested regularly. Many are unaware they are living with the virus, because in most people, there are no symptoms – until it is far too late.
Jake’s case, wherein flu-like symptoms showed within the first few weeks of infection, is extremely rare. The first few weeks are when the body first tries to respond to the virus. Symptoms go away on their own and are so similar to the flu that very few assume the symptoms are from HIV.
But in majority of people – 91% of the recorded HIV cases in the Philippines – the symptoms do not even show at all. So many live with the virus for years, not knowing they are infected. Most find out they had been living with HIV, only when it turns into full-blown AIDS – when the immune system becomes too weak to fight off infection that they develop illnesses.
When Jake first realized he was HIV positive, he tried to contact his former partner to let him know, and to tell him that he believes he got it from him. But by then, the latter had blocked him from social media and all forms of communication.
Does he think his former partner knows he is infected with HIV? “I don’t think that he knows.”
There is no telling how many other youth in the Philippines are unaware they are living with HIV and having sex – unknowingly infecting others.
But advocates have a general idea.
According to the AIDS Epidemiology Modeling, around 62% of the estimated newly-infected are coming from the 15-24 age group, which means the Philippines is diagnosing only around 23%-50% of that 15-24 group. So many others are living with the virus, that without treatment, is slowly but steadily breaking down their immune systems.
They’re having sex, Figuracion said, and that’s a fact. It’s not about stopping them from having sex, it’s about making sure they’re safe.
Troops out to battle
Figuracion said FPOP, which has 22 chapters and clinics across the country, has now invested in adolescents programs: making sure they are providing them testing services, teaching them about HIV prevention, and for those who need it, treatment.
In their office, there’s a huge map plastered across a wall, next to the staircase. It’s massive, and detailed, down to tiny streets across the city. It’s used to map where their target market is, where the youth are. Their strategy is detailed, analytical – Figuracion like a general sending troops out to battle.

“We want to know where they converge, where they meet, which geographical sites are the hot spots. Where do they usually hang out?” Figuracion, said gesturing to the map.
In this case, the troops are other youth. Figuracion’s soldiers are what he calls “peer counselors.”
“Rather than hiring nurses or doctors doing the groundwork, we really have to empower their peers. Most of our volunteers are also members of the young key population,” he said.
Their theory is that the youth will be more comfortable talking about sex with other youth. The same goes with other at-risk populations: for MSMs or transgenders for instance, peer counselors are also members of those groups.
There’s a master list or directory of volunteers who report to the office from time to time to grab some condoms or lubricants, and who sometimes even lure target clients to the headquarters in exchange for free contraception. Once there, they become more open to take an HIV test.
The strategy is especially effective with key populations, like MSMs, who are “discrete and closeted.”
“There are those whom you really just can’t tell. From the looks, you wouldn’t know they are guys who are into guys,” Figuracion said with a shrug. “So our strategies work because they’re comfortable with each other and they can really bring people in (to get tested). Or they can bring us to their community and we do that sometimes.”
And as in any battle, the soldiers go far deep into the war zone, even going to beach parties popular with the youth like Labor Day festivities in Boracay – notorious for beach parties, booze, and sex – where peer counselors distribute condoms, and FPOP makes HIV tests available.
They even make condoms and lube readily available for orgies, when they hear they’re happening.
“Sometimes, there are those that come here to ask for condoms, not just one or 3 packs, but one or two boxes. That’s fine, no problem. We don’t have to lecture during orgies. Nothing like that.”
He adds, “But just to make the condoms available in the center table is already a good sign, a reminder to be safe. Just handing the condom out – it’s already like an advocacy.”

Peers
There is some good news. The government agrees HIV prevention among the youth is a priority. The Department of Education is open to age-appropriate sex education. And even Catholic Churches are advocating for HIV prevention – although the strategy they promote is abstinence, rather than the use of condoms.
Darlene de la Peña, a DOH health educator from the Region 6 office, said they are getting a lot of support from headquarters, so they are able to help organizations like FPOP.
“Actually, our funding comes mostly from our central office that is based in Manila and we are now giving more logistics to our partner organizations just like the FPOP when it comes to our testing. Like giving them enough supply of testing kits as well as other logistics that would help in the prevention of transmission of HIV-AIDS,” De la Peña said.
DOH itself gives FPOP boxes and boxes of condoms and lubricants to distribute. But there’s still a lot of work to be done.

Figuracion said there’s a need to engage all stakeholders – from the education sector to parents at home – to train teachers on comprehensive sex education, to fight stigma, and to get the youth to access testing and treatment when needed. He said they also need to highlight that treatment is available and free for those with PhilHealth, since less than half of HIV positive individuals in the Philippines actually seek treatment.
It is also deeply crucial for local government units across the country to do their part.
“It’s really the local government units that we want to move right now. That’s legislating ordinances to have an HIV program city per city, province per province, and then towns per towns. We want to make sure that the local chief executive knows the numbers and also has resources to actually provide for the program,” he said.
There’s also a need to change the current law, which dictates that minors under 18 need parental consent to get tested for HIV – which is a challenge, since many LGBT youth cannot even tell their parents about their sexuality.
The goal is this: that 90% of those who are HIV positive should know their status, that 90% of those who know their status should actually get treatment, and that 90% of those who are on treatment should be virally suppressed.
“If we can achieve that, then it is not far to curb the epidemic very soon.” But for now, “the epidemic is everywhere,” he said. “It does not discriminate on age. It does not discriminate on sex. Not even on social class or economic class.”
HIV myths
Jake said he has told only a handful of people of his status, his most inner circle, but that his relatives have an inkling he is living with HIV.
“They told every single person that I have HIV or I have AIDS. So every time that I drink using their glasses, or every time that I stay in their house, it broke my heart because I saw those plates I use – they actually have it thrown away.”
It’s a laughable fear – to contract HIV by sharing utensils or even through saliva – since the only ways HIV can be passed on from one person to another, is through blood, sexual fluids, and breast milk, primarily through unprotected anal or vaginal sex, sharing needles or syringes, or from mother to child during pregnancy or breastfeeding. Even oral sex has very little to no risk of HIV transmission.
But even basic HIV information like this, is not known to many. Jake hopes this would change, that more youth would read up on HIV and get tested, that talking about safe sex need not be taboo.
‘They told every single person that I have HIV or I have AIDS. So every time that I drink using their glasses… it broke my heart because I saw those plates I use – they actually have it thrown away.’
– Jake*, on the stigma he experienced living with HIV
The truth is, the future is not so bleak for Jake – because he found out early.
Since his diagnosis, his dream to work at sea stays alive.
Jake is currently in touch with Positibong Marino Philippines Inc or PMPI, a support group and network of HIV positive seafarers, which fights for the rights of people living with HIV to be able to work at sea.
An international convention to which the Philippines is a signatory says that if an HIV-positive seafarer has a very low likelihood of disease progression, are stabilized on medication, and have no requirements for frequent surveillance, the seafarer is considered to be “able to perform all duties worldwide within designated department and may participate in long voyages.” Jake should thus be allowed to work as a seafarer.
“I actually lost hope because I didn’t want to push it because I thought it was a waste of money, waste of time. I just wanted to work, just locally. But they told me, ‘No. Push it. We’ll help you. We’re here. We are going to help you. You’re going to work onboard and we’re going to help you.’”
And while he will need to take medications for the rest of his life to suppress the virus, like anyone who is infected, antiretroviral treatment in the Philippines is readily available. This is another little-known fact: medication for those living with HIV is free for those with PhilHealth.
At just 21, he very much looks forward to a long life ahead of him. He said he no longer regrets anything. While it initially felt like the universe had played a trick on him – he contracted the virus the one time he slept with a guy he met online – the stars did align when he found out about his positive status soon after.
He urges the youth to secure their futures.
“There’s nothing to worry about. Early detection can prolong lives so it’s important to know their status. If they’re negative, they have to be able to know how to stay that way in order to be safe. Then if they know that they are positive, then they’ll be able to know how to undergo medication to prolong their lives.”
“So before it worsens and before it become AIDS, as long as it’s still HIV, they still have all the possibilities that they could live their lives longer.” – Rappler.com
*Names have been changed for the protection of the individual
Top photo from Shutterstock; all other photos by Dyl Tolentino for Rappler
Add a comment
How does this make you feel?

![[PANOORIN] May ‘silent epidemic’ sa Pilipinas?](https://www.rappler.com/tachyon/2023/12/silent-epidemic-dec-7-2023.jpg?resize=257%2C257&crop_strategy=attention)



There are no comments yet. Add your comment to start the conversation.