SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.
![[ANALYSIS] When should we relax the lockdown?](https://www.rappler.com/tachyon/r3-assets/612F469A6EA84F6BAE882D2B94A4B421/img/92EED83215A341DE8296BDC2C6B44708/when-to-relax-the-lockdown-may-1-2020.jpg)
I. Testing disparity should not decide our post-lockdown scenario
The Philippines’ post-April 30 scenario came out on April 24 (revised on April 30), and the following day we became aware of the IATF’s considerations for continuing or relaxing the enhanced community quarantine (ECQ).
According to the Facebook post that came from the UP COVID-19 Pandemic Response Team, the IATF’s did not differ much from their projections, and both relied on the measurement of factors that are related to COVID-19’s reproductive number (R, a measure of the epidemic’s behavior in the population).
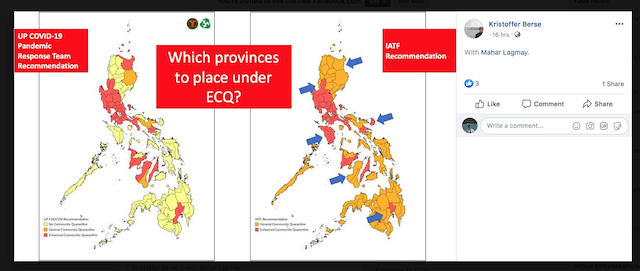
The number R has appeared in many simulations performed on this epidemic’s trajectory locally and internationally, and it tells whether the lockdown has been effective (R decreased from pre-lockdown value) or not. Now, R, is being used on the provincial level to decide whether or not to continue with the ECQ (if the epidemic is still raging, R has a value more than 1) or relax it (the epidemic is halting, R has a value less than 1).
The problem is, the basis for estimating R, DOH testing data (as of April 27), displays disparities: most COVID-19 cases occur in the provinces where the testing centers are located!
Figure 2 reveals this by region (more cases in regions with testing centers).
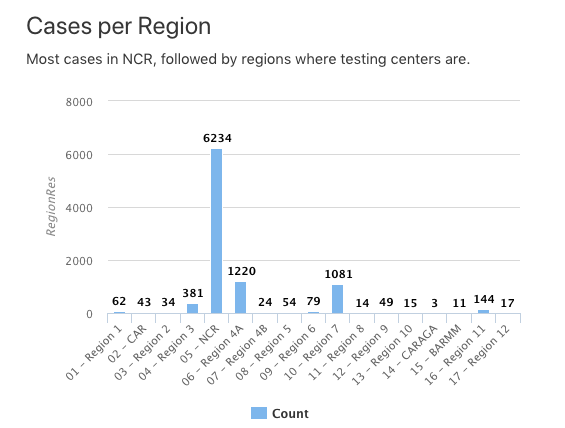
Figure 3 shows it by province in Region VI (more cases in Iloilo where the testing center is).
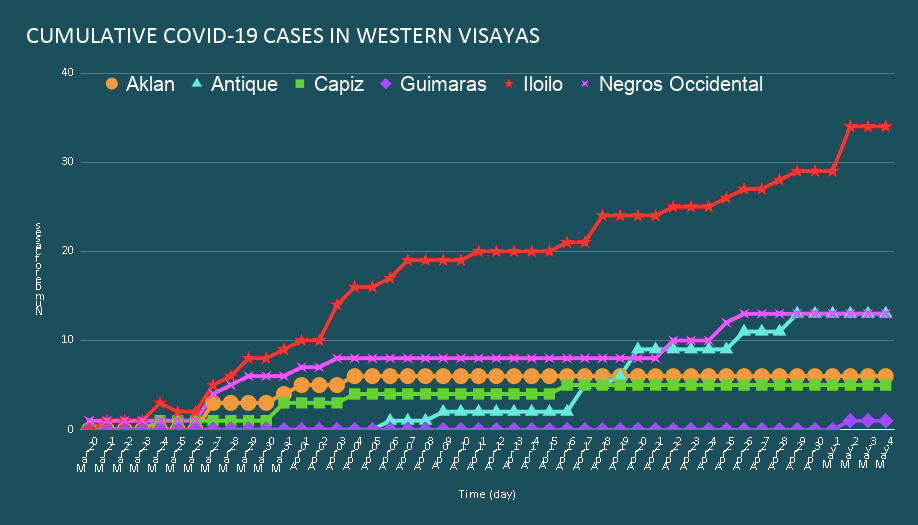
There is an eye-popping correspondence between the location of testing centers, where COVID-19 cases cluster, and the continuance of ECQ in certain provinces per the IATF recommendation; peril arises when the discontinuance of ECQ is recommended where few cases are being observed which may reflect not a lack of cases but rather a lack of testing.
A police officer on night duty encounters a drunkard, who appears to be searching for something under a streetlight. “What are you looking for?” asks the officer. “My car keys,” replies the drunkard. The two search together under the streetlight. “Are you sure you lost them here?” “No, I lost them in the park.” “So why are you looking for them here?” “Because this is where the light is.”
This illustrates the drunkard’s search principle, whereby a drunk and his helpful but uninformed friend search only where it is easiest to look. For COVID-19, the testing centers are the streetlights, and this principle can have a disastrous effect when the search for cases “under the streetlight” is then used in the decision to relax the lockdown where it is dark. Therefore, our recommendation is to test, test, test and bring testing equality to all provinces especially since the decision to continue or relax ECQ requires provincial testing data. Otherwise, we can try to unearth testing disparities and address them accordingly, for example, how arduous is it to bring samples from far away provinces to testing provinces and get results (make it easier!), how prejudiced are testing provinces against other provinces (no prioritization!), etc.
The molecular (RT-PCR) vs. rapid (antibody) testing debate continues to rage on but we think that these two modes of testing complement each other. We made recommendations on how many tests must be performed in Quezon City based on projections that we have been constantly refining and planned the ramp up of RT-PCR testing capacity. We’ve discovered how difficult it is.
Consider, one RT-PCR test costs about P3,500 overall (including tests reagents, equipment, manpower and PPEs, before prices started climbing) and each recovering patient may be tested more than once. To acquire the equipment and reagents is becoming more and more difficult as countries try to ramp up their own testing per the WHO recommendation. To comply to the biosafety required, and to find and train the manpower to carry out RT-PCR testing have been bottlenecks in testing center accreditation.
On the other hand, determining one’s exposure to the virus by detecting the body’s response to it with rapid (antibody) tests is cheaper (about 1/5th of RT-PCR) and quicker (15-30 minutes vs days). The (much maligned) accuracy of these rapid tests may be improved by repetition, and the interpretation of the results can be aided by testing twice between 8-10 days (paired tests). We have even recommended saving on tests by pooling samples. In the end, we must will ourselves to test massively and extensively if post-lockdown decisions are to be driven by data. Lack of testing is lack of data.
II. Alternatives to estimate R with
In the absence of molecular or rapid testing, there are other sources of information that can give an estimate R to help with the decision. One is hospital admission – these reflect how rapidly the epidemic is progressing, in terms of the depletion of hospital resources. However, the information we gleaned tells us that the data is incomplete and not yet ready for primetime.

Another is prescription utilization – sales by pharmacies of medicines to alleviate the symptoms of COVID-19. It follows that there will be more and more prescriptions filled in a runaway epidemic compared to one that is coming to a halt. Again, however, a pharmacy registry, where this data resides, does not (yet) exist here. Both these out-of-reach prospects underscore the need for better and inter-operable health information systems.
Finally we turn to a potential indicator of R that is less costly and more accomplishable: contact tracing. Contact tracing finds the people that an infected person may have passed the virus to (these are the “contacts”). We think that if an epidemic is still expanding, the list of contacts will be expanding too, reflecting R. One would think that this list of contacts is affected by the testing disparity, and yes it is, however, since untested “probable” and “suspected” COVID-19 cases will also be traced, especially those with symptoms of COVID-19 and perhaps those diagnosed using other modalities such as X-ray and CT scan, then the disparity is mitigated.
We developed a contact tracing tool for use in the National Center for Mental Health (NCMH) to keep track of their outbreak, piloted it and discovered that people who are notified of the existence of the tool are very willing to self-report their contact with a COVID-19 case. Thus contact tracing can be aided by self-reporting. Individuals who have had an encounter with a COVID-19 case can report, trace their contacts, and monitor their own symptoms.
Overall, contact tracing activities are like a net trying to catch the cases, and the expansion of the size of that net mirrors R. If there is a central contact tracing tool available in every province they can quickly get an estimate of their R by analyzing the data contributed by all of their contact tracers and citizens. Then they will have a good idea whether or not to relax their ECQ.
All over the world, we are seeing that large scale contact tracing is becoming a tool to track the epidemic and decide on easing up on quarantine. Contact tracing is a win-win-win in cost, effort and potential effectiveness. – Rappler.com
Romulo de Castro is a Balik Scientist of the DOST-PCHRD and the Director of the newly-established Center for Informatics (CFI) at the University of San Agustin (Iloilo City).
Salvador Eugenio Caoili is a professor at the Department of Biochemistry and Molecular Biology, College of Medicine, University of the Philippines Manila, where he serves as a faculty mentor for their MD-PhD (Molecular Medicine) Program.
Vena Pearl Bongolan is an associate professor at the Department of Computer Science of UP Diliman, where she teaches modeling, dynamical systems, and computational differential equations.
Add a comment
How does this make you feel?
There are no comments yet. Add your comment to start the conversation.