SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.


Since the outbreak of the COVID-19 pandemic early this year, the Philippine General Hospital (PGH) has received and continues to receive donations of various kinds.
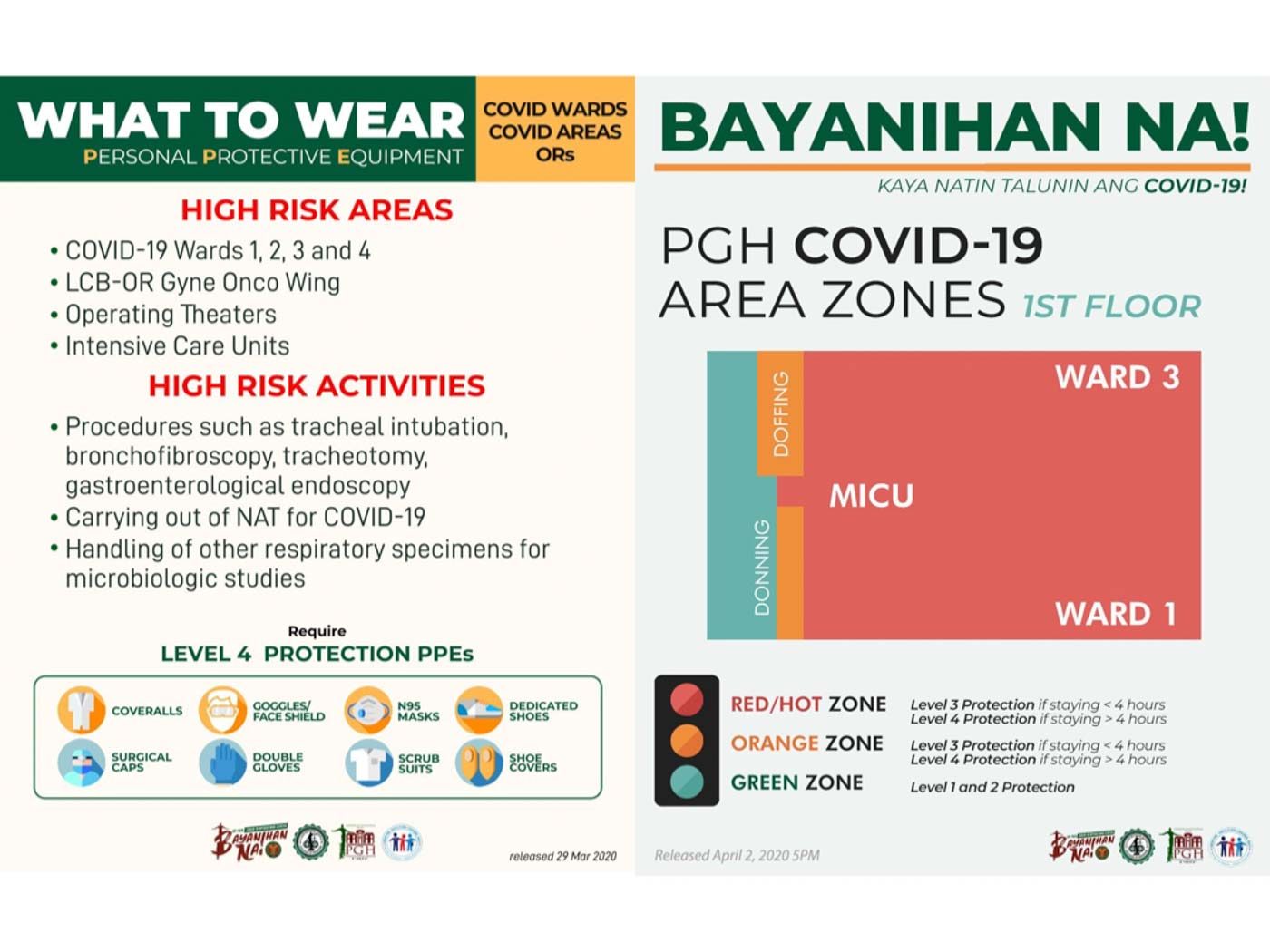
These include Personal Protective Equipment (PPE) for our healthcare workers who serve as frontliners. PPEs are barriers that healthcare workers should wear on top of their scrub suits. These are needed to reduce the risk of transmission of COVID-19 from the patients to the HCWs or healthcare workers. A “complete” PPE set typically includes a gown or coverall, gloves, mask, eye protection, head cap, and booties.
Forecasting PPE usage in a COVID-19 referral center
In February 2020, we started to see and admit patients who were suspected of having COVID-19, classified as Persons Under Investigation or PUIs. We put on or “don” these PPEs whenever we examine PUIs. After leaving the patient’s room, we would then remove or “doff” the PPEs.
Suppose a doctor and a nurse need to see a PUI at the emergency room, they would use a total of two PPE sets. Once admitted, this patient would be monitored at least once every work shift, with 3 shifts in 24 hours. Thus, 6 to 8 PPE sets are needed each day, for doctors and nurses alone.
When additional tests are needed (e.g., blood test, EKG, and X-ray), each healthcare worker who performs a procedure will need to don PPE. Easily, the usage would be about 12 sets of PPEs per day for each patient. Multiply that by 14 days, which is the usual duration of hospital stay of COVID-19 patients, and we would therefore need at least 168 PPE sets from admission to discharge.
The cost of providing adequate PPE for healthcare workers also needs to be considered. The Department of Health (DOH) recently procured one million PPE sets worth P1.8 billion. Using these figures, the total cost of PPE for just one patient will be about P300,000. Even if the cost were halved, the amount is still staggering.
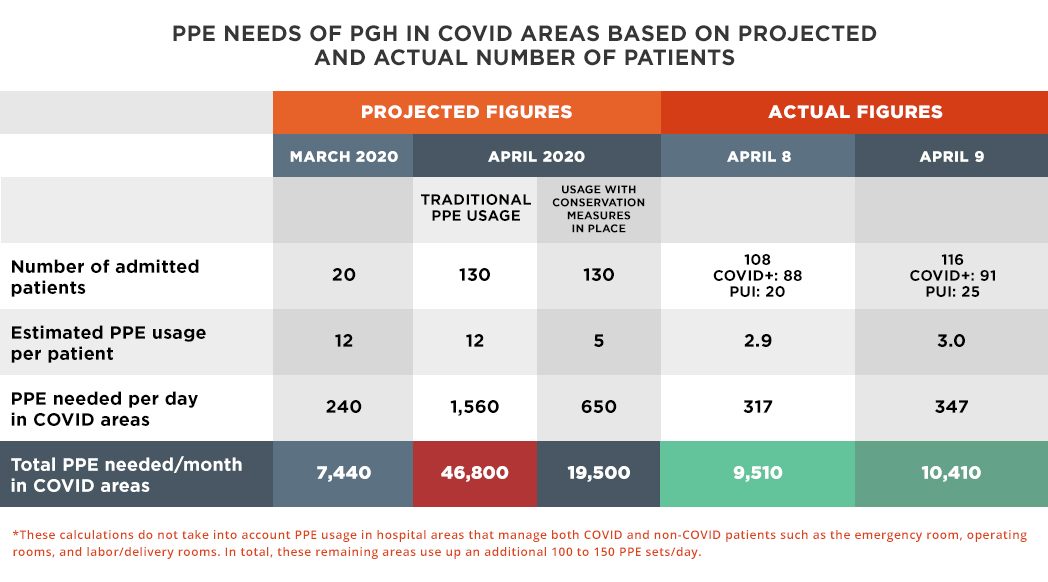
As the number of PUIs in PGH started to increase, we saw the need to procure more PPEs. When we initially projected treating 20 COVID-19 patients for March 2020, we estimated that we would need almost 8,000 sets for the whole month.
But on March 22, the DOH announced on national TV that PGH was chosen to be a COVID-19 referral center, and that we committed to have 130 patients. Based on the prevailing PPE usage, we would need to build a stockpile of 46,800 PPE sets, and do so quickly. This was clearly ambitious if not impossible. Hence, together with the PGH community, we have been developing ways to conserve our PPEs.

PPE conservation strategies at the PGH
Here, we outline the ways through which we have managed to streamline our PPE use and reduce wastage, while at the same time ensuring the safety of our healthcare workers.
1. Cohorting of COVID-19 patients
Cohorting means patients with the same diagnosis are placed together in a common area. It is a great, feasible strategy for hospitals that manage a large number of patients. Since all the patients in this set-up are COVID+, the issue of transmissibility between patients is eliminated.
In PGH, we have designated 4 COVID wards to safely accommodate 22 COVID+ patients each, maintaining a reasonable distance of 2 meters between beds of intubated patients (i.e., on a mechanical ventilator) and one meter between beds of non-intubated patients. We currently have 4 such big cohort wards, which can accommodate up to 88 COVID patients altogether. In the private floors of the hospital’s central block, a similar strategy was used, in which all COVID+ patients are admitted in assigned wings of the 5th and 6th floors.
Cohorting all confirmed COVID-19 patients in wards leads to a significant reduction in the required number of PPEs per shift. Nurses and doctors on duty can move efficiently from one bed to the next, just by changing their outer gloves after each patient (Note: healthcare workers wear two layers of gloves) and performing hand hygiene frequently. It is an acceptable way of patient bed allocation, as long as good ventilation is assured, necessary bed distance is allotted, and precautions are observed during usage of common toilet facilities and daily interaction between patients.
In the old system, if we don one PPE set per COVID+ patient, we would have needed 264 PPEs per day in this 22-bed ward alone or 7,920 sets per month. In this new cohort system, we allocate based on the number of staff per ward. We now use only about 60 PPE sets per day or 1,800 sets per month per ward. This translates to a 75% reduction in PPE usage.
PUIs are more resource-intensive and more difficult to manage from the PPE perspective.
While awaiting their COVID-19 diagnostic test results, they need to be protected using fresh PPE because of the possibility that they are not COVID+ after all. To solve this, we have designated PUI wards, and in these areas, healthcare workers are given outer gowns that they put on top of their PPE, every time they interact with a patient. Each PUI is allocated 3 to 5 outer gowns per day. The total number of PPE sets used by healthcare workers remains the same, since only the outer gown and gloves are shed with each patient interaction.
2. Zoning of COVID and non-COVID areas
At the outset, the Hospital Infection Control Unit of PGH divided the hospital into COVID and non-COVID areas. The COVID areas were further divided into Red, Orange, and Green zones.
We have created a PPE scheme (now casually known to all PGH employees and volunteers as PPE Levels 1, 2, 3, 4) to determine risk categorization and appropriate PPEs for every role, every department, every staff, every area, hopefully distinguishing exactly what PPE is needed for all. Nothing can be left to chance. Everybody is afraid, but we cannot operate on fear and PPEs are finite resources. All need to be protected but in a reasonable, science-based manner, adhering to sound principles of infection control.
A creative group of physicians work on producing easy-to-understand posters to educate staff on the proper use of PPEs. These materials are disseminated through social media, Viber groups, and displayed in tarpaulins at relevant areas in the hospital. These guidelines have reduced unnecessary use, for example, of N95 masks when medical masks would suffice.
3. Assigning dedicated personnel for COVID wards
To perform its role as a COVID-19 referral center, PGH completely overhauled its human resource allocation. We don’t work by departments anymore. The COVID areas are staffed by physicians and nurses from the entire hospital, unified by a centralized mechanism under the lead of pulmonologists and infectious disease specialists.
The number of healthcare workers needed to care for each COVID-19 patient or PUI has not been reduced: patients are seen by two to 5 doctors per day, one nurse per shift, one nurse assistant, and paramedical support as necessary (phlebotomist, radiation technician, EKG technician, dialysis nurse, and others). Nurse:patient ratio is maintained at no lower than 1:2 in the intensive care units (ICUs) and 1:7 or 1:8 in the wards.
Non-COVID wards and ICUs of PGH continue to run with a skeleton workforce, managing a markedly reduced number of non-COVID patients since elective admissions have been put on hold. The staffing of COVID and non-COVID zones do not overlap.
Healthcare workers are assigned to work in only one area during their 8-hour shift. This means they could safely wear the same PPE for 8 hours, changing their outer gloves as often as needed and performing frequent hand hygiene. Staff in the COVID zones would come in for 7 consecutive days, followed by a rest period of two weeks, after which the duty cycle repeats itself. There are 3 teams in all.
4. Improving operational efficiency
To improve the efficiency of stocking PPEs and monitoring their usage, adjacent COVID wards, ICUs, and hospital wings have been grouped together, and each group has a centralized area where PPEs are supplied. These demarcated floor spaces or rooms are identified as donning zones. A separate doffing zone is also identified for each unit. Typically, two to 3 wards share donning and doffing zones.
Safety officers – volunteer doctors and staff from different departments – are present to guide and assist healthcare workers whenever they don their PPE just before entering a COVID zone, and once more, when they doff, after leaving the COVID ward or ICU. Once daily, the safety officers of all units accomplish a Google form to keep track of PPE usage and request for replenishment from the hospital’s supply division.

PGH set up a central command system to manage the hospital’s COVID-19 operations. A consultant is in charge of the distribution of PPEs to all sectors of the hospital, so that everyone gets just what they need, in both COVID and non-COVID zones. If we see a trend of overuse in one ward, we investigate and correct wastage. On the other hand if an area calls out for a need to augment specific PPEs, they are addressed immediately. Constant awareness of remaining hospital inventory is also crucial, considering that there may be delays in procurement of specific PPE, and the quantity and quality of PPE from donors have been variable.
5. Earning commitment of healthcare workers
Donors of PPE often ask: How many PPE sets are needed in a day? In PGH, healthcare workers in COVID areas are allocated two PPE sets when they go on duty, allowing them to take a break, if necessary, midway through their shift. Thus, to get a reasonable estimate, you need to know the number of healthcare workers in moderate to high-risk areas for 24 hours, then double that number.
Having said that, the need to conserve PPE is emphasized to staff during their orientation and training for donning and doffing. If each person would take a break on the 4th hour of duty, this would mean removing the entire PPE set and changing into new ones. And the usage will very easily double or triple. When we started off, the initial reaction of physician and nursing staff was that they could not possibly stay in their PPE suits for the eight-hour shift: “Impossible!”
We have asked our staff to prepare well, physically and mentally. They are encouraged to eat their meals before or after their shift, and to keep themselves hydrated. Before donning PPE, they are reminded once more to empty their bladders. Adequate ventilation of work stations is ensured to minimize perspiration and fatigue. At the rest station, water and snacks are readily available. We’ve observed that as healthcare workers get used to their work routine, more and more nurses and doctors are taking the extra effort to stay in their PPEs and sacrifice to the 8th hour without changing. Staff who need to urinate frequently are encouraged to use diapers.
Perhaps the most difficult rule for staff is that no mobile phones are allowed inside COVID zones. Phones are left in lockers and staff are instructed to inform loved ones that there will be no means of communication for eight hours. Hospital communication is through landline, local hospital network, and walkie-talkie. Socializing and unnecessary talking are discouraged, and physical contact of PPEs is prohibited.
6. Assigning personnel to reprocess select PPE
We have been recycling goggles, which are decontaminated and cleaned after use. Specific nursing staff have been assigned to do this task. Cleaners and janitors also wear proper PPE. They are part of the allocation for N95 masks and eye protection. They use coveralls made of heavy-duty material, which allows for washing and safe reuse.
Projections and results
As PGH nears the end of its second week as a designated COVID-19 referral center, we have been able to reduce PPE usage to less than 350 PPE sets/day in our COVID zones, or an average of 3 PPE sets/day for every COVID+/PUI patient (See table). If we add PPE usage in areas that manage both COVID and non-COVID patients (e.g., emergency room, operating rooms, labor/delivery rooms), which ranges from 100 to 150 PPE sets/day depending on the number of patients seen, the entirety of PGH presently uses approximately 500 PPE sets daily.
As we admit more COVID+/PUI patients, we foresee that this figure may reach 700, but most probably no higher. We are monitoring the effects of these conservation strategies on our healthcare workers with vigilance.
The impact of our measures cannot be overstated, and we hope that by sharing our best practices, this may serve as a guide for other hospitals in the country who face the same dilemma of rational PPE allocation.
We continue to accept all PPE donations, and we would like to profusely thank all our donors. We also thank all PGH COVID-19 frontliners for cooperating despite challenging circumstances, and for adhering to hospital policies for the greater good and everyone’s safety.
Because of all of you, we are more certain there will always be enough PPEs to protect all healthcare workers with each new day, as PGH continues to serve and give hope to Filipino patients throughout this pandemic. – Rappler.com
Dr. Regina P. Berba is an associate professor at the University of the Philippines College of Medicine. She is head of the PGH Hospital Infection Control Unit. Dr. Ronnie E. Baticulon (@ronibats) is also an associate professor at the UPCM and a pediatric neurosurgeon in PGH. UP Press published his book of essays in 2019.
For comments and queries, please email rpberba@gmail.com.
Add a comment
How does this make you feel?
There are no comments yet. Add your comment to start the conversation.