SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.

MANILA, Philippines – During a disaster, it is difficult to count deaths and to ascribe them to the disaster or to some other cause. Deaths can also be prevented or caused by the responses to the disaster (the so-called disaster after the disaster).
As hospitals worked at full capacity and regular health services were disrupted during the first two years of the pandemic, the Philippines had around 95,577 more deaths per year compared to the average of the previous five years. These deaths were not only from COVID-19 but from other health conditions for which people were unable to access timely treatment.
Conversely, there were fewer deaths from certain conditions, possibly the unintended consequences of the preventive measures against COVID-19.
From our analysis of the 2021 report of the Philippine Statistics Authority (PSA), the top 10 causes of death that exceeded their baseline number of expected deaths (average of 2015-2019) during the pandemic were:

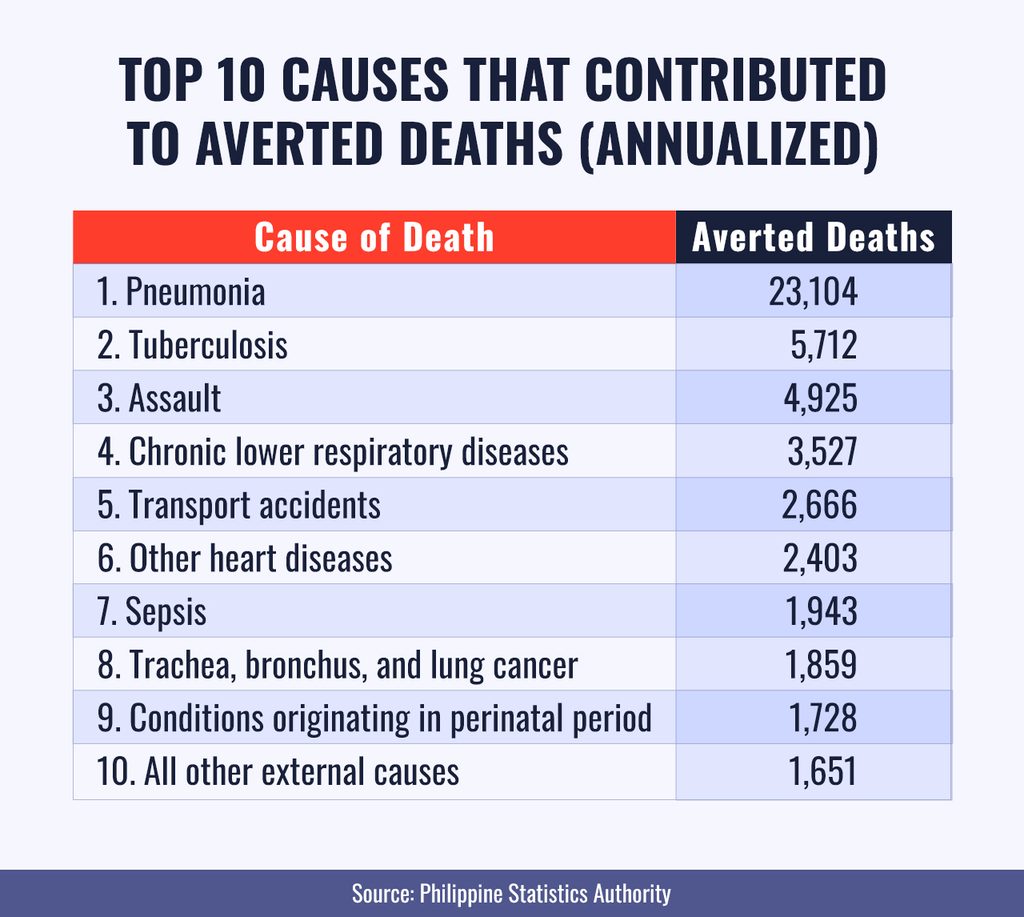
Meanwhile, the top 10 causes of deaths averted (meaning, less than the expected number of deaths) were:
To determine how the number of deaths during the pandemic compares to the number of deaths under “normal” circumstances, we used the concept of excess mortality.
Excess mortality is computed by subtracting the expected from the actual number of deaths. The number of expected deaths is the average deaths during the five years previous to the pandemic – that is, the average annual number of deaths from 2015 to 2019. Determining the excess mortality allows us to identify the causes of deaths that probably either resulted from the pandemic or from the response to it. Some deaths were also averted as unintended consequences of the pandemic interventions, such as masking.
Estimates from the World Health Organization (WHO) show a large increase in excess mortality globally. It reached a total of around 14.9 million in 2020 to 2021, when the pandemic was at its peak. In the Philippines, the deaths were 40,147 lower than expected in 2020 and 213,984 higher in 2021. This number puts the Philippines at the upper 28% of lower middle-income countries in terms of excess mortality.
Based on the WHO estimates, the net number of deaths is 173,837 over two years; this estimate is within 9% of the PSA’s estimates. While the PSA’s estimates are entirely based on death certificates, the WHO’s estimates are partly modeled. However, the PSA estimates are within the margin of error of the WHO’s estimates.
The increase in deaths due to specific causes is a commentary on the types of people who were at risk during the pandemic: the very old and the very young. From 2020 and 2021, there were a higher number of deaths due to non-communicable diseases (NCDs) compared to the average deaths in the previous five years. Most excess deaths were due to vascular diseases like ischemic heart disease (heart attacks), cerebrovascular diseases (strokes), and hypertension. Endocrine diseases, particularly diabetes, also experienced an increase in deaths. These NCDs require regular treatment and checkups and the multiple lockdowns could have caused disruptions in patients’ ability to access these services.
In addition, there was also an increase in the number of deaths from malnutrition, most probably from the loss of income and from food insecurity. Although we don’t have an age breakdown, we know that very young malnourished patients are at higher risk of death compared to older patients.
Meanwhile, there were fewer deaths related to communicable diseases – the so-called diseases of poverty – specifically, pneumonia, tuberculosis, and chronic respiratory diseases. Deaths from these diseases could have been prevented through the same protective measures that were effective in lowering the risk of COVID-19 infection, like masking and social distancing. Also, deaths from diarrheal diseases and sepsis could have been decreased from improved hygiene practices.
While deaths due to communicable diseases generally decreased, there was an alarming rise in deaths from HIV, which could also be related to difficulties in accessing antiretroviral therapy during the lockdowns.
With most of us staying at home during the lockdown periods, there were also fewer deaths from injuries as a whole, including transport accidents, drowning, and assaults. On the downside, there were higher deaths due to injuries that frequently occur at home, such as falls, self-harm, and accidental poisoning.
Notably, a large part of excess deaths were due to unknown or unclassified causes, which could be due to difficulties in ascertaining the actual cause of death.
Lockdowns delayed hospital care
Circumstances behind the pandemic could have aggravated certain comorbidities. These include diseases such as hypertension, ischemic heart disease, and cerebrovascular disease.
Dr. Divine Agustin, a cardiology fellow, said it was likely that patients were unable to access hospital services due to the fear of catching a COVID-19 infection. She noted: “In the period of 2020 to 2021, hospital capacity was so full at the time that patients were even afraid to seek medical care. [The] Filipino culture or health seeking behavior could have played a role as well. Filipino patients were fearful that they would be left alone in the hospital with no family member with them.”
Dr. Steven Villaraza, a neurologist, noted a similar phenomena: “At the time, we saw more patients with cerebrovascular disease or stroke coming in with bleeding. This kind of stroke is usually more complicated and severe, which could lead to death. Patients with milder forms of stroke would tend to delay hospital care and they ended up consulting with us weeks later after the stroke had happened. I believe these patients were hesitant to proceed to the hospital for their condition.”
In our analysis, certain cancers were also found to have contributed to an increase in excess deaths. Dr. Abigail Tud, an orthopedic oncologist, noted that during the period of 2020 to 2021 there was a surge in the number of patients being referred for metastatic bone disease, or cancers from other organs such as breast and prostate cancer that had spread to the bones. These were often accompanied by breaks in the diseased bone, a condition called pathologic fractures, which typically occurred in cancers in advanced stages. As lockdowns occurred, cancer patients might have been unable to undergo proper monitoring not only because of their fear of going to the hospital and transportation constraints, but also because hospitals struggled with sustaining diagnostic services like lab tests and diagnostic scans.
“As strict lockdowns took effect in 2020, supply chain disruptions led to difficulties in procuring certain laboratory reagents essential for performing tests to evaluate cancer patients. These caused significant diagnostic and treatment delays for patients,” Dr. Tud noted. Overall, patients who were previously diagnosed with cancer were unable to follow up on their condition. This had the greatest impact on patients with more aggressive malignancies, such as lung and renal cancers. At the time, patients suspected of having cancer required screening for detection, but many such services were likewise difficult to access, especially for patients with financial constraints.
Averting deaths from other causes: A boon for some patients
In contrast, deaths from certain diseases were averted. Decreased deaths from pulmonary causes – such as pneumonia, influenza, tuberculosis, and chronic respiratory diseases – were noted in 2020 to 2021. Dr. Claire Orden, a pulmonologist, explained that patients had less exposure to other infections due to social distancing and the wearing of face masks.
“I also noticed that our patients with chronic respiratory diseases were more careful and mindful of their exposures. I believe this lessened their risk of exacerbations, complications, and death,” Dr. Orden noted. Patients with chronic lung conditions usually die of secondary respiratory infections. As such, even pulmonary tuberculosis patients benefited from these lowered risks of exposure.
Death from traumatic injuries lessened during the time of 2020 to 2021. Dr. Sally Mae Abelanes, an emergency medicine physician, noted that she was seeing fewer vehicular accidents at the time. “We usually see more trauma or vehicular accident patients during Fridays. But as lockdowns forced people to stay at home, we saw a significant decrease in those cases and, subsequently, deaths related to them,” Dr. Abelanes explained.
Attention is needed for mental health
Although it did not make it to the top 10 causes of excess deaths, deaths related to self harm (suicides) were notably higher by 1,545 cases (59% increase) during the period of 2020 to 2021. During this time patients had limited access to psychiatric services. Dr. Fatima Campaña, a psychiatrist, believes that circumstances surrounding the pandemic caused an overall decline in mental health for some individuals. “The feeling of isolation was hard for some. Due to limited manpower and beds as a result of the COVID surges, we were limited in our capacity to admit patients,” Dr. Campaña explained.
Suicide patients tend to be brought to the emergency department. Dr. Abelanes, the emergency medicine physician, noted; “We usually have to try to investigate the causes of these intentional self harm cases. Patients may not necessarily have pre-diagnosed psychiatric conditions. But it is likely the pandemic has caused a kind of mental health decline. Some patients lost their jobs or were unable to maintain their relationships. Successful suicides were only a handful, however, but a lot of parasuicides or suicide attempts were noted in the emergency department.”
Limited testing capacity early in the pandemic may have missed COVID-19
Although data suggests that excess deaths were apparent in 2020 to 2021, some specialists believed that some of these were still caused by COVID-19 but the diagnosis was likely missed. Dr. Roberto Noche III, a cardiology fellow, noted that diseases such as ischemic heart disease, hypertension, stroke, and diabetes are risk factors for COVID-19 mortality.
“Early in the pandemic, hospitals struggled to routinely test patients. I suspect these patients that died with cardiovascular disease could have COVID, but it was difficult to make that diagnosis without a test. Some of those who expired were untested, which could underestimate our COVID death numbers. In general, COVID puts everyone at greater risk for cardiovascular disease so it can all overlap,” Dr. Noche explained. If testing was limited during these times, excess deaths due to COVID-19 could have been underestimated.
Excess deaths are likely the tip of the iceberg
The analysis of excess deaths gives us but a glimpse of how our nation performed during the pandemic. The years of 2020 to 2021 were difficult for the health system. It was a time in which quality information about COVID-19 was sparse. The accurate reporting of deaths is a critical indicator in determining whether or not our health system responded appropriately. If patients were unable to seek medical care before they expired, the causes of some deaths may be vague or non-specific. It is, thus, possible and probable that the excess deaths caused by the pandemic have been underestimated.
Lessons learned
Both excess and averted mortality are summary measures of the impact of the pandemic and our response to it. We need to qualitatively and quantitatively investigate the context and causes behind both types of mortality.
First, the SARS-CoV-2 virus itself can cause death in a small percentage of cases (global average case fatality rate = 1.06%). It is probable that many COVID-19-related deaths were prevented through the combination of interventions that we implemented: lockdowns, masking, improved hygiene, hospital treatment, vaccinations, and oral antivirals. However, old age, the presence of comorbidities, and being immunodeficient increases this risk. Ensuring a higher vaccination rate and wider access to oral antivirals among these subpopulations could have minimized their risk of death.
Second, some of the interventions we utilized against the pandemic were double-edged swords. On the positive side, aside from preventing COVID-19 deaths, they could also have prevented deaths from other causes. For example, masking could explain the averted mortality from pneumonia, influenza, TB, and chronic respiratory diseases. Better hygiene practices could explain the decreased mortality from diarrheal diseases and sepsis.
On the negative side, some interventions could also have induced additional deaths. Lockdowns, the near shutdown of transportation, and the focus of hospital resources on COVID-19 patients could have prevented patients with acute conditions from accessing needed care, prevented patients with chronic conditions from acquiring the maintenance treatment that they needed, and intensified feelings of depression, leading to suicides.
Third, systems to guarantee continuity of emergent, acute, and long-term care need to be reviewed. Emergency transportation for acute conditions could be secured, and supply chains for maintenance medications for chronic conditions, like HIV, could be strengthened.
Fourth, looking at excess deaths beyond COVID-19 could help us calibrate the use of these interventions in the future. For example, lockdowns could be more localized and be shorter.
Finally, the ability of our systems of death certification, particularly, the abilities to count and to determine the causes of death need to be improved. The reports need to be more complete, accurate, timely, and relevant.
The pandemic is not over yet. We have a set of tools that we can use to manage future surges. But knowing the tradeoffs that each tool brings allows us to choose more wisely which ones to use and how to use them to achieve the best outcomes with the least cost and the least harm. – Rappler.com
John Q. Wong, MD, MSc; Carlo Yao, MD, MBA; and Jemuel Joshua Austria are from EpiMetrics Inc., a public health research institution focused on the achievement of health equity through rigorous and creative conception, execution, translation, and communication of health systems and policy research.
Add a comment
How does this make you feel?
There are no comments yet. Add your comment to start the conversation.