SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.
![[ANALYSIS] COVID-19: The difference in death rates](https://www.rappler.com/tachyon/r3-assets/612F469A6EA84F6BAE882D2B94A4B421/img/097C90819E1B4763B0653D47C1FE2A05/article-2-march-24-2020.jpg)
Editor’s note: A longer version of this article was first published on Medium on March 10, 2020. It is being reposted with the author’s permission. Watch and read the transcript of Pueyo’s interview with Rappler.
READ: Part 1 | How many cases of COVID-19 will there be in your area?

The coronavirus is already here. It’s hidden, and it’s growing exponentially.
What will happen in our countries when it hits? It’s easy to know, because we already have several places where it’s happening. The best examples are Hubei and Italy.
Fatality rates
The World Health Organization (WHO) quotes 3.4% as the fatality rate (% of people who contract the coronavirus and then die). This number is out of context so let me explain it.
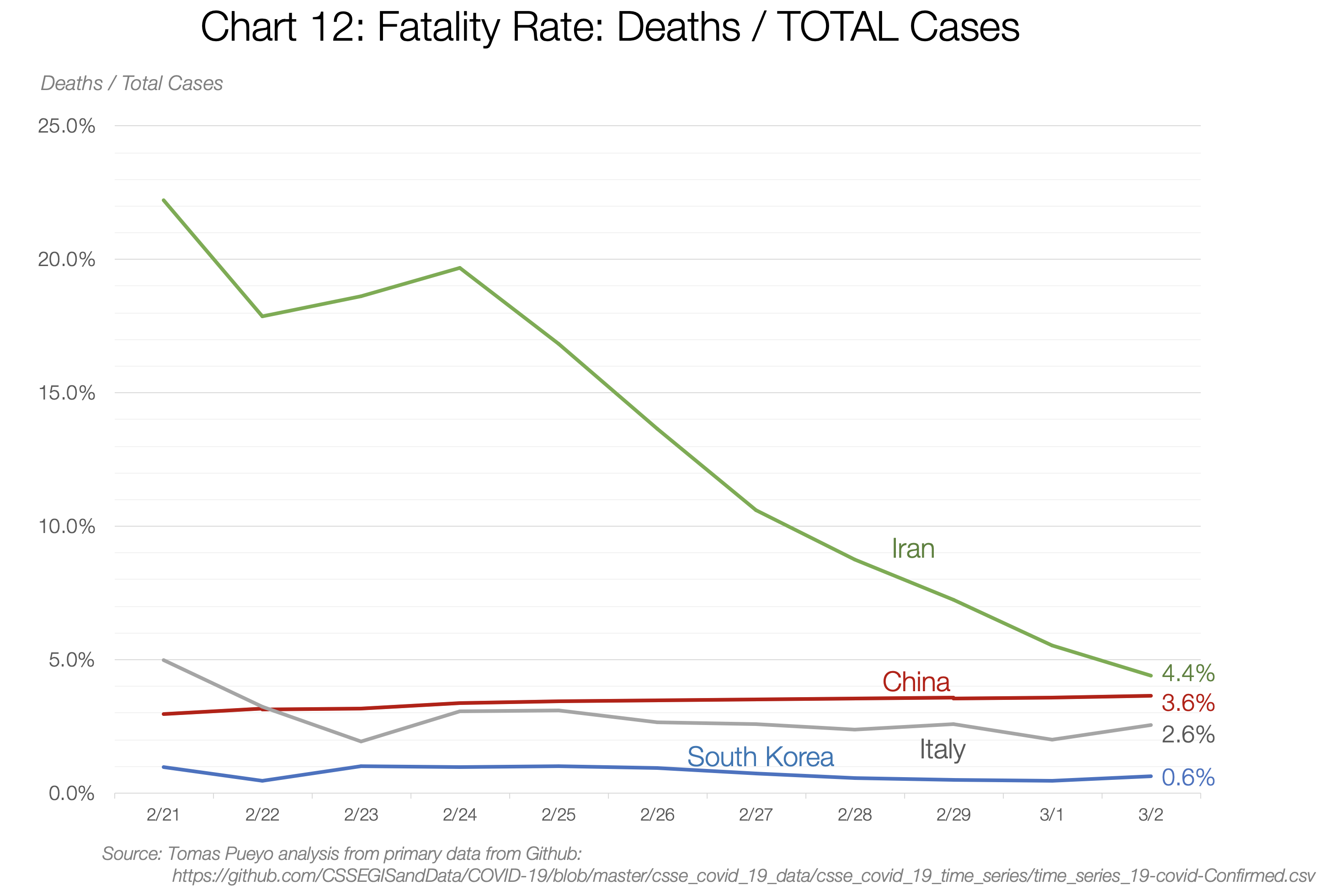
It really depends on the country and the moment: between 0.6% in South Korea and 4.4% in Iran. So what is it? We can use a trick to figure it out.
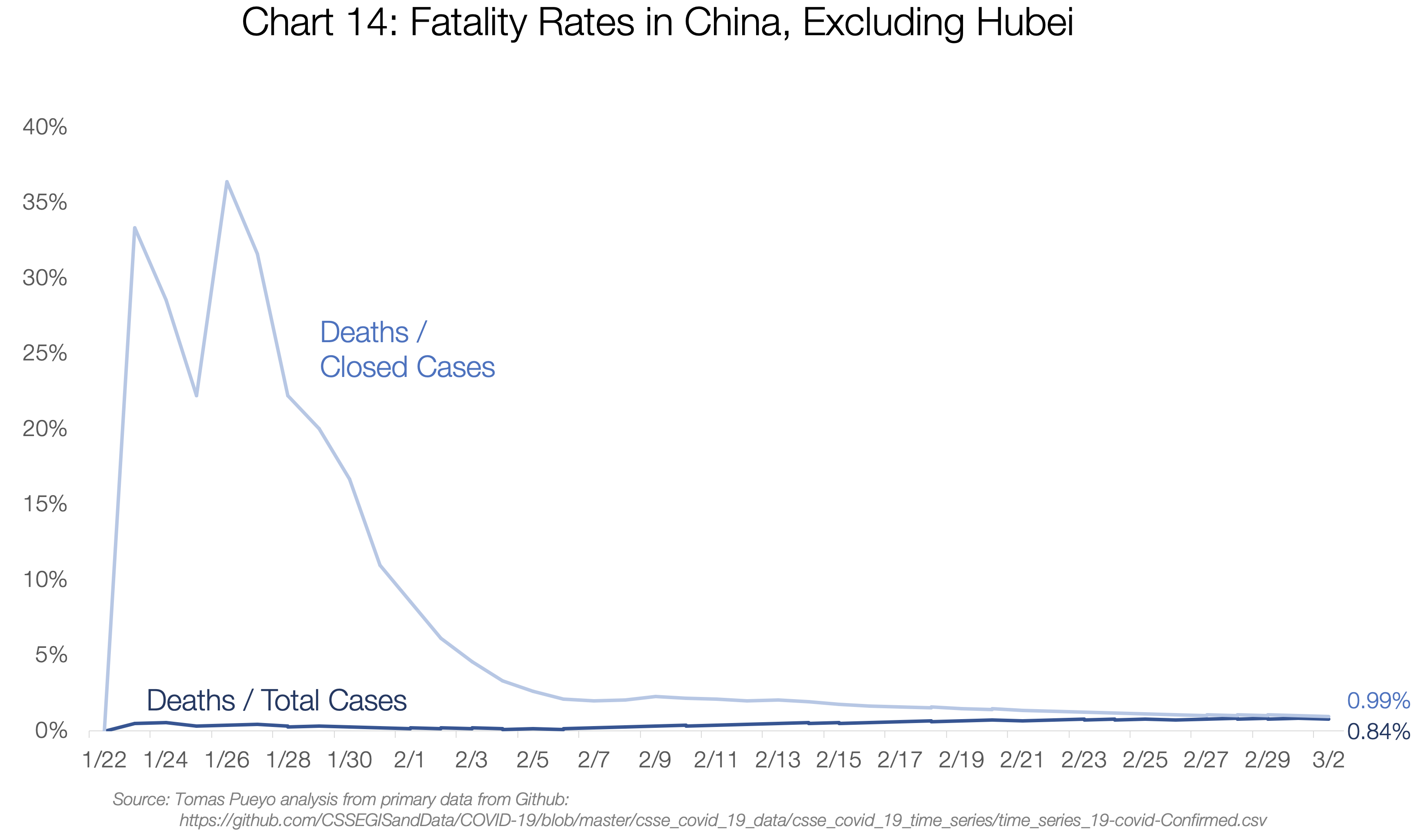
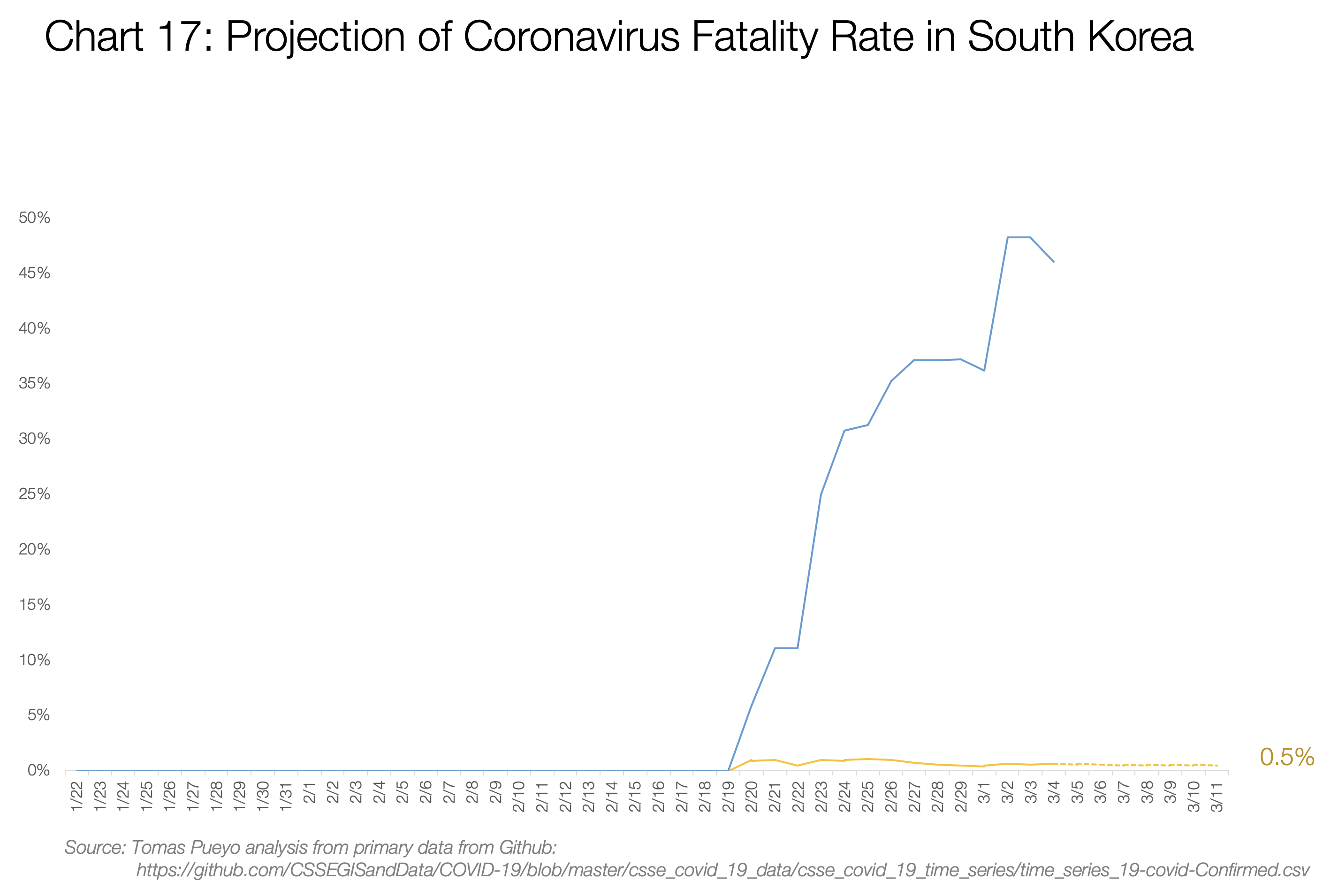
The two ways you can calculate the fatality rate is Deaths/Total Cases and Deaths/Closed Cases. The first one is likely to be an underestimate, because lots of open cases can still end up in death. The second is an overestimate, because it’s likely that deaths are closed quicker than recoveries.
What I did was look at how both evolve over time. Both of these numbers will converge at the same result once all cases are closed, so if you project past trends to the future, you can make a guess on what the final fatality rate will be.
This is what you see in the data. China’s fatality rate is now between 3.6% and 6.1%. If you project that in the future, it looks like it converges towards ~3.8%-4%. This is double the current estimate, and 30 times worse than the flu.
It is made up of two completely different realities though: Hubei and the rest of China.
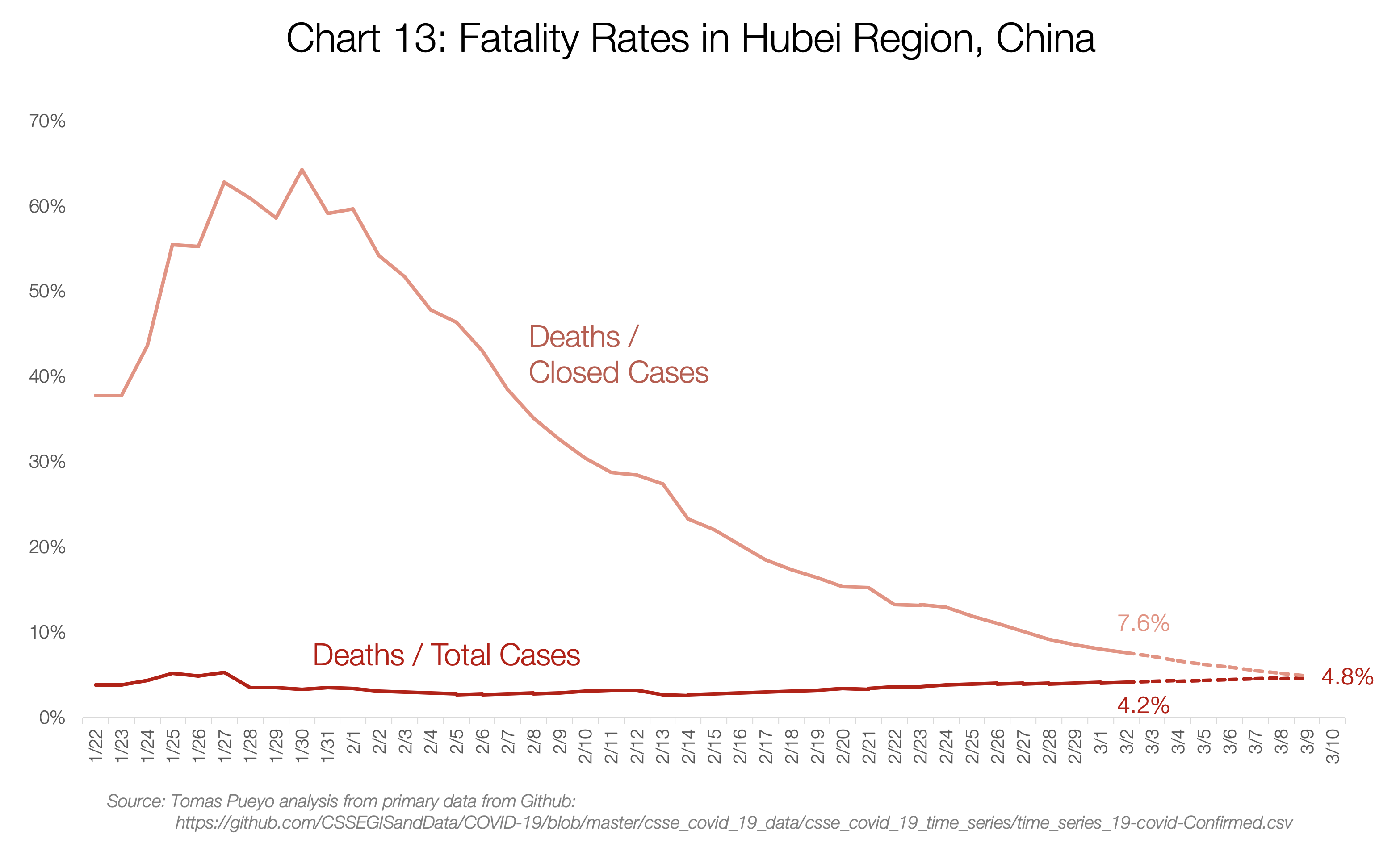
Hubei’s fatality rate will probably converge towards 4.8%. Meanwhile, for the rest of China, it will likely converge to ~0.9%:
I also charted the numbers for Iran, Italy, and South Korea, the only countries with enough deaths to make this somewhat relevant.
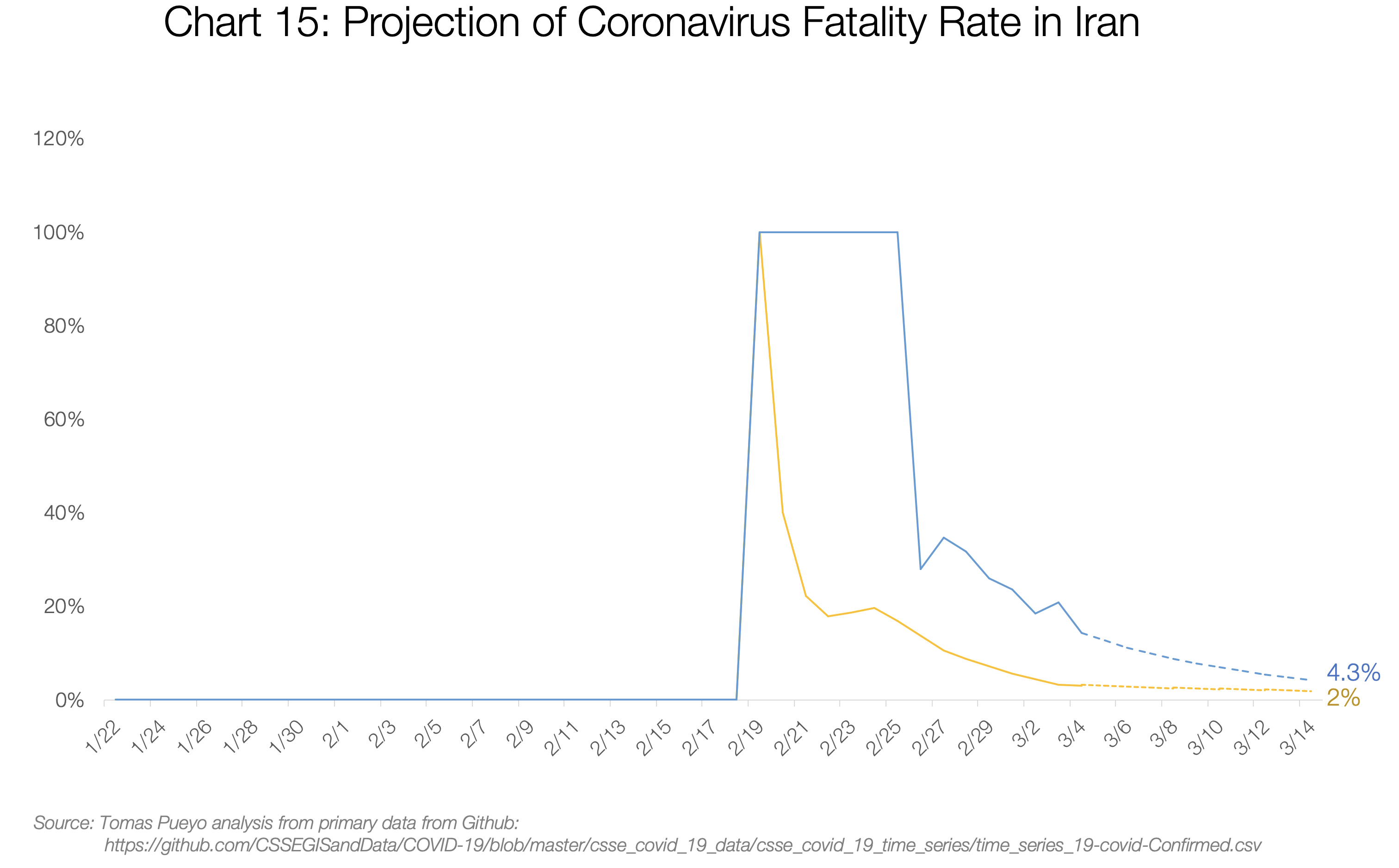
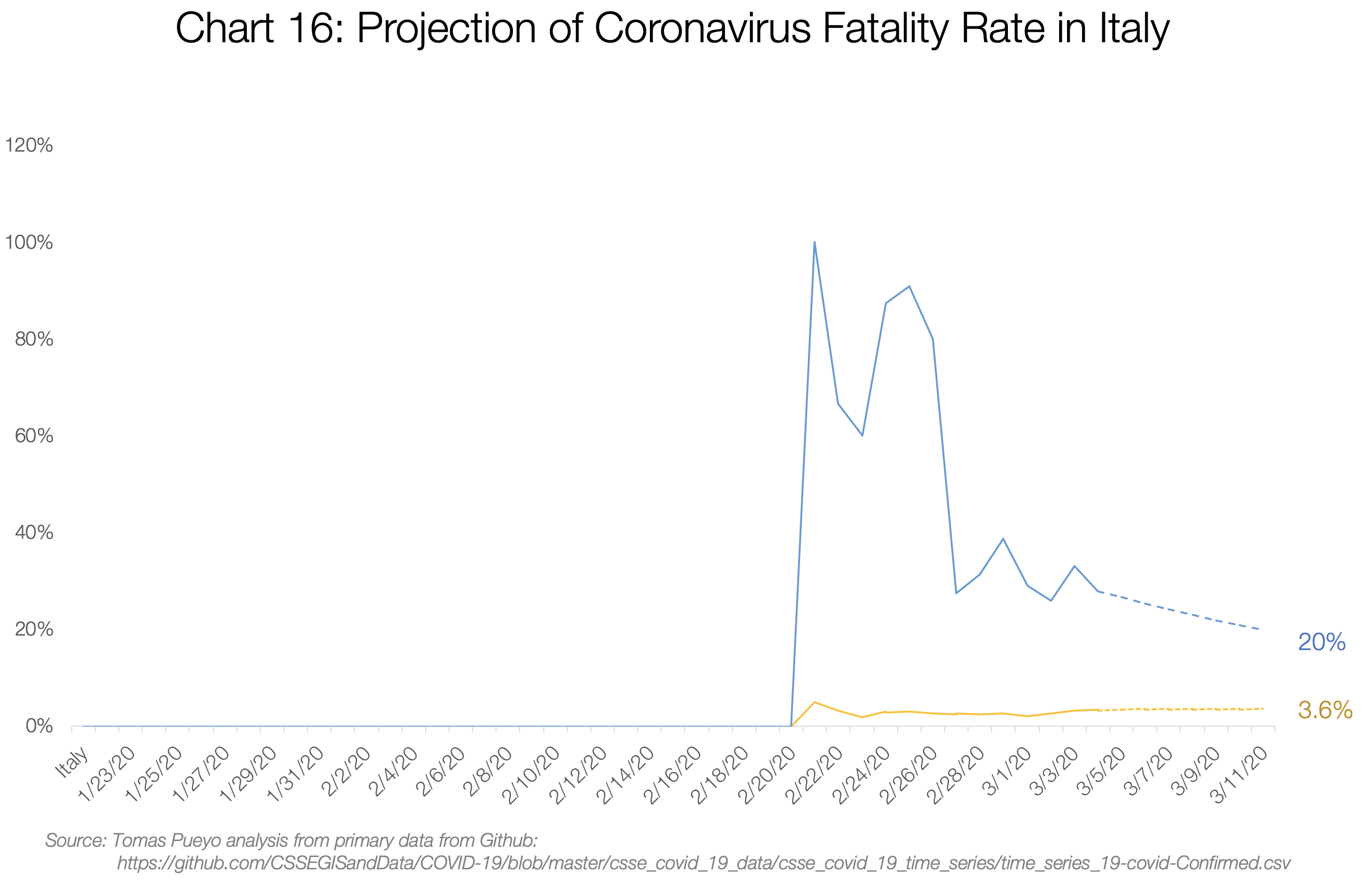
Iran’s and Italy’s Deaths / Total Cases are both converging towards the 3%-4% range. My guess is their numbers will end up around that figure too.
South Korea is the most interesting example, because these two numbers are completely disconnected: deaths / total cases is only 0.6%, but deaths / closed cases is a whopping 48%. My take on it is that a few unique things are happening there.
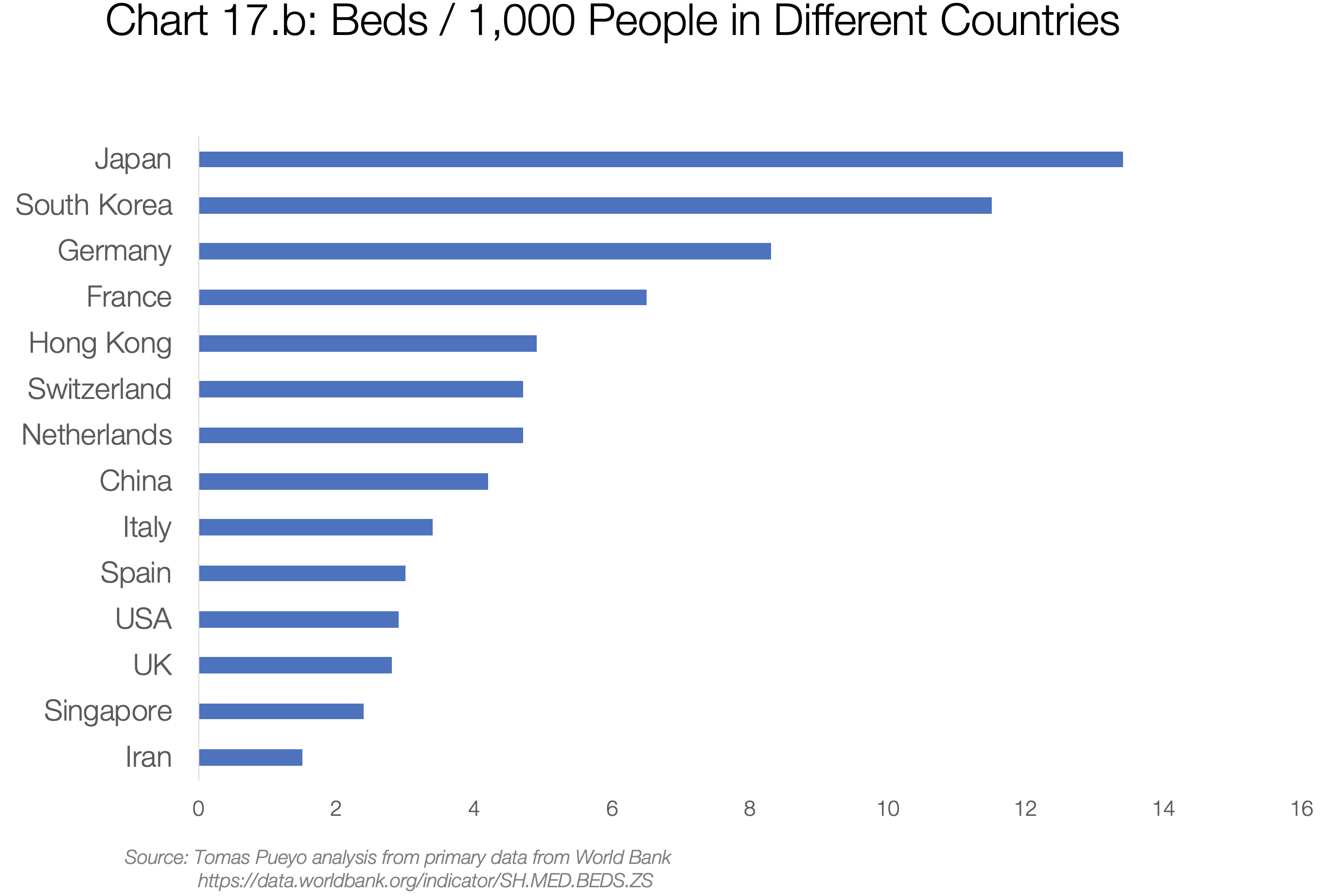
First, they’re testing everybody (with so many open cases, the death rate seems low), and leaving the cases open for longer (so they close cases quickly when the patient is dead). Second, they have a lot of hospital beds (see chart 17.b). There might also be other reasons we don’t know. What is relevant is that deaths/cases has hovered around 0.5% since the beginning, suggesting it will stay there, likely heavily influenced by the healthcare system and crisis management.
The last relevant example is the Diamond Princess cruise: with 706 cases, 6 deaths and 100 recoveries, the fatality rate will be between 1% and 6.5%.
Note that the age distribution in each country will also have an impact: Since mortality is much higher for older people, countries with an aging population like Japan will be harder hit on average than younger countries like Nigeria. There are also weather factors, especially humidity and temperature, but it’s still unclear how this will impact transmission and fatality rates.
This is what you can conclude:
- Excluding these, countries that are prepared will see a fatality rate of ~0.5% (South Korea) to 0.9% (rest of China).
- Countries that are overwhelmed will have a fatality rate between ~3%-5%
Put in another way: Countries that act fast can reduce the number of deaths by a factor of ten. And that’s just counting the fatality rate. Acting fast also drastically reduces the cases, making this even more of a no-brainer.
So what does a country need to be prepared?
What will be the pressure on the system
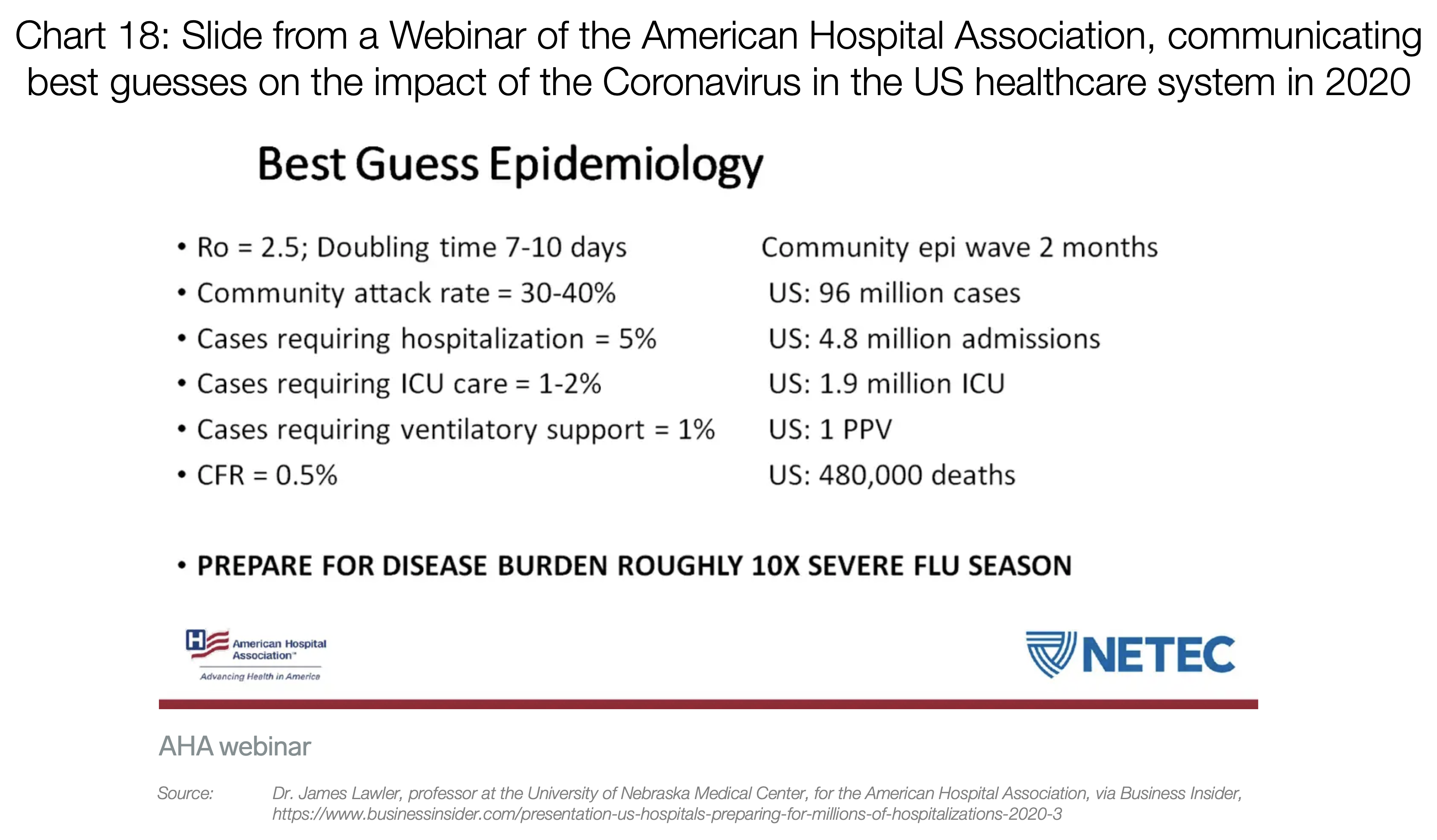
Around 20% of cases require hospitalization, 5% of cases require the Intensive Care Unit (ICU), and around 2.5% require very intensive help, with items such as ventilators or ECMO (extra-corporeal oxygenation).
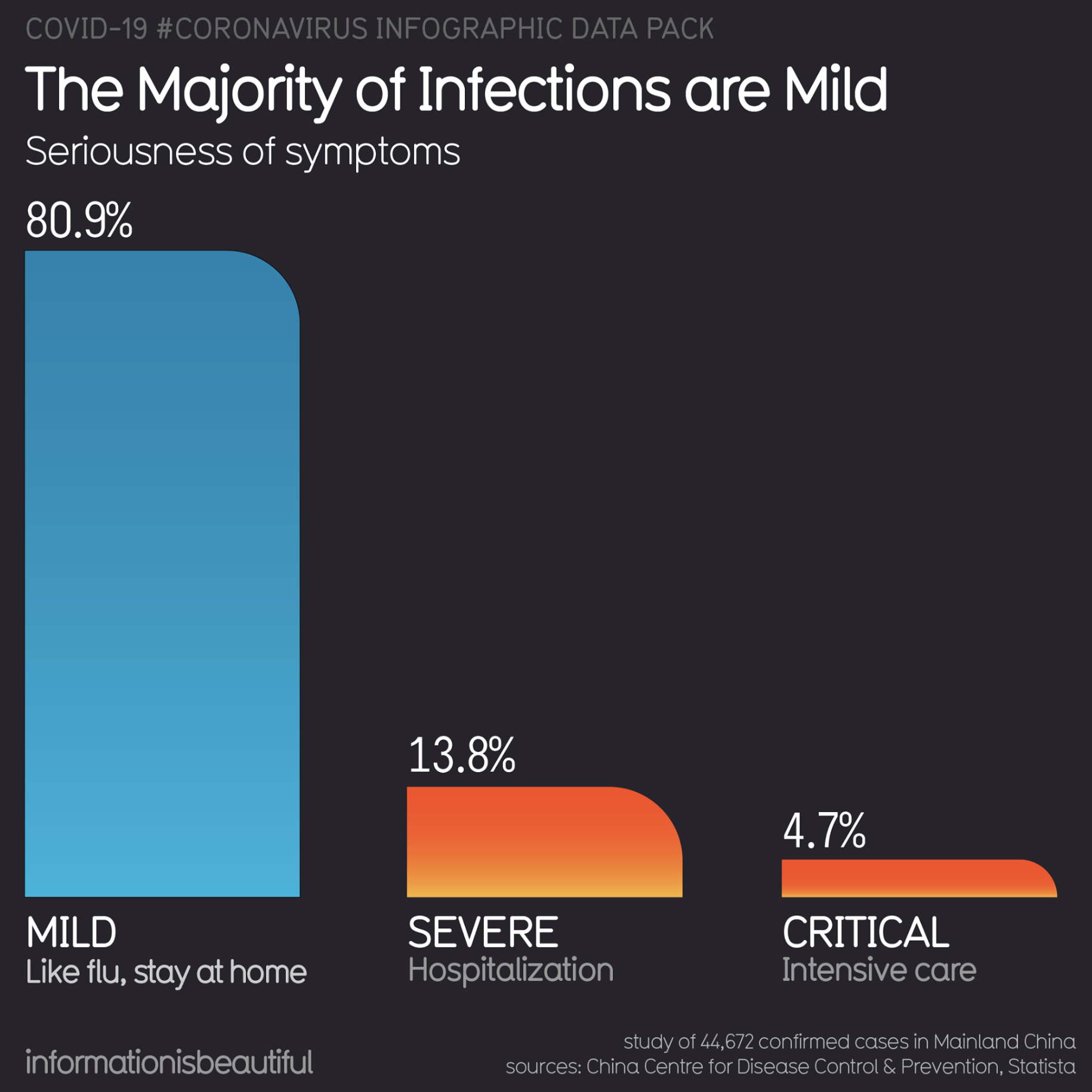
The problem is that items such as ventilators and ECMO can’t be produced or bought easily. A few years ago, the US had a total of 250 ECMO machines, for example.
So if you suddenly have 100,000 people infected, many of them will want to go get tested. Around 20,000 will require hospitalization, 5,000 will need the ICU, and 1,000 will need machines that we don’t have enough of today. And that’s just with 100,000 cases.
That is without taking into account issues such as masks. A country like the US has only 1% of the masks it needs to cover the needs of its healthcare workers (12M N95, 30M surgical vs. 3.5B needed). If a lot of cases appear at once, there will be masks for only two weeks.
Countries like Japan, South Korea, Hong Kong or Singapore, as well as Chinese regions outside of Hubei, have been prepared and given the care that patients need.
But the rest of Western countries are rather going in the direction of Hubei and Italy. So what is happening there?
What an overwhelmed healthcare system looks like
The stories that happened in Hubei and those in Italy are starting to become eerily similar. Hubei built two hospitals in 10 days, but even then, it was completely overwhelmed. Both complained that patients inundated their hospitals. They had to be taken care of anywhere: in hallways, in waiting rooms…
From a well respected friend and intensivist/A&E consultant who is currently in northern Italy:
1/ ‘I feel the pressure to give you a quick personal update about what is happening in Italy, and also give some quick direct advice about what you should do.
I heavily recommend this short Twitter thread. It paints a pretty stark picture of Italy today
Healthcare workers spend hours in a single piece of protective gear, because there’s not enough of them. As a result, they can’t leave the infected areas for hours. When they do, they crumble, dehydrated and exhausted. Shifts don’t exist anymore. People are driven back from retirement to cover needs. People who have no idea about nursing are trained overnight to fulfill critical roles. Everybody is on call, always.
Francesca Mangiatordi, an Italian nurse that crumbled in the middle of the war with the Coronavirus
That is, until they become sick. Which happens a lot, because they’re in constant exposure to the virus, without enough protective gear. When that happens, they need to be in quarantine for 14 days, during which they can’t help. Best case scenario, two weeks are lost. Worst case, they’re dead.
The worst is in the ICUs, when patients need to share ventilators or ECMOs. These are in fact impossible to share, so the healthcare workers must determine what patient will use it. That really means, which one lives and which one dies.
All of this is what drives a system to have a fatality rate of ~4% instead of ~0.5%. If you want your city or your country to be part of the 4%, don’t do anything today. – Rappler.com
*Tomas Pueyo is a Silicon Valley entrepreneur and behavioral psychologist who specializes in exponential growth. He wrote the Medium post, “Coronavirus: Why You Must Act Now,” which was read by tens of millions of people around the world.
Add a comment
How does this make you feel?
There are no comments yet. Add your comment to start the conversation.