SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.
![[ANALYSIS] Fighting the COVID-19 pandemic: How do we ‘heal as one?’](https://www.rappler.com/tachyon/r3-assets/612F469A6EA84F6BAE882D2B94A4B421/img/666245C43C5D48E39CB6D4CA009DF335/thought-leaders.jpg)
We were not alone in underestimating the COVID-19 threat. With every country inextricably linked to China, where this disease started percolating, the rest of the world was similarly caught flat-footed.
But while our health systems are not as advanced as other countries, we could have done a lot better.
We Filipinos are no strangers to disasters. Regular exposure to various natural hazards have built innate resilience in our people.
What’s different here is that the threat concerned – unlike in other crises – is invisible. But this is not the first time we have managed a threat like this either. We had experience with SARS in 2006. Health authorities did not do badly in containing that outbreak.
So what went wrong? And how do we move on from here?
Comprehensive, holistic approach
The first thing we need to do is go back and review well-established workflows for disaster risk reduction and management: prevent, prepare, respond, recover.
Looking at this problem from this comprehensive and holistic lens is critical because you want to avoid cures that are worse than the disease and you want to mitigate future vulnerability to this threat.
The fact that our medical frontliners are forced to go to work without personal protection equipment and the lack of coordination in the way the quarantine or lockdown protocols were implemented shows just how much we failed with respect to the first two phases of this workflow.
To help us move forward, it is crucial to assess and acknowledge where we failed and provide a clear accounting of where the gaps are. Transparency and humility on the part of the political leadership is key to helping this country heal as one. It is also critical to enable everyone who can help to jump in and help out more effectively.
Let me go through some of the things that were missed one by one.
Step 1: Assess risk vulnerability, prevent, mitigate
Disaster management experts will tell you that the first critical step to preventing a crisis is to assess the hazard (in this case a disease outbreak), determine level of exposure and vulnerabilities to the hazard, and plan ways to mitigate risks in relation to a particular threat or hazard.
The formula goes this way: risk = hazard x exposure x vulnerability.
They also stress this: every dollar spent on prevention and mitigation saves US$6 or more in losses.
We failed in this critical part of the workflow when Philippine authorities failed to accurately assess potential exposure and vulnerability to COVID-19, even though we have been pivoting more closely towards China politically and economically in recent years. A red flag should have been raised when the first case, a tourist from Wuhan, was confirmed on January 30 this year.
The fact that the first and second cases were able to go through various local airports undetected should have pushed the government to level up action. It was clear from that point that surveillance efforts were not enough and that the level of risk was significant.
For instance, hiring more people to do contact tracing, and investing in mechanisms to strengthen quarantine measures would have prevented those with the disease from infecting others. Instead of making sure that this is done, President Duterte dismissed the outbreak as “nothing to be scared about.”
The health department recently did a callout for volunteer data gatherers to help with contact tracing. This might be too late for areas in Metro Manila where local transmission is evident but may still be helpful for areas in the country where cases reported involve travelers from other places.
Here, effective risk communication is paramount. The Presidential Communications Operations Office (PCOO) should focus on communicating the nature of the threat and how local governments can prevent further exposure to it in their respective areas, instead of dismissing critics’ concerns.
Step 2: Plan, test plans, prepare to respond
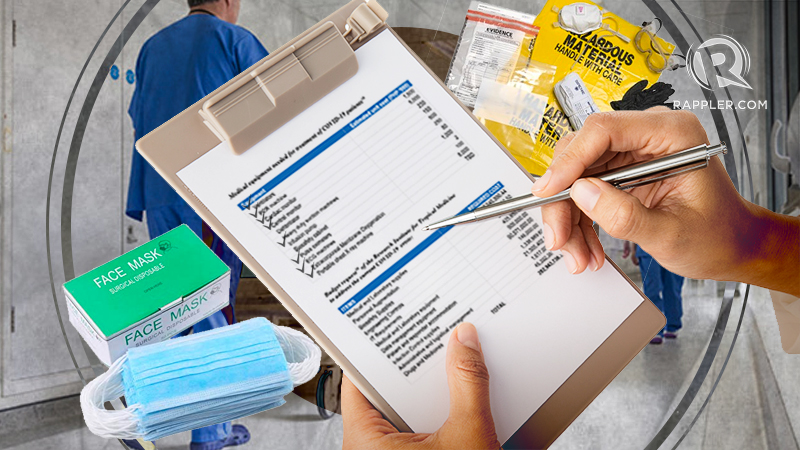
The first case was reported January 30. The first death from local transmission due to COVID-19 was confirmed March 9. The month in between these two dates could have been the golden window for what disaster managers call the preparedness for response phase. Having a checklist of needs and things to do helps at this point.
Instead of patting themselves on the back, the Department of Health could have used this window to sound the alarm and ensure that local disaster managers were oriented on what’s unique about this threat and what needs to be done to manage it. Workflows and functional capabilities should have been assessed and tested at this stage.
Supplies needed for emergency response should have been procured. We could have ordered personnel protective equipment and ventilators at this point, given the amount of time it takes to get these manufactured and shipped out.

Step 3: Respond, get people out of harm’s way, help those in need
Given that local transmission is obviously happening already, it makes sense to make people stay at home in the meantime. With less people moving around, the likelihood of the virus spreading uncontrollably and exponentially beyond the capacity of the health system is minimized.
But what are indicators the quarantine is working? Lockdowns, according to the World Health Organization (WHO) are not enough to defeat the coronavirus. Finding those who are sick and isolating them, finding their contacts and isolating them, too, should be the focus.
Granular, up-to-date data on how the disease is spreading is critical to effective response. This is where a testing strategy helps, according to former health secretary Manuel Dayrit. Testing helps those fighting to stop the disease see how it is spreading.
Beyond counting the sick and the dead, we also need real-time tracking of needs on the ground such as PPEs, ventilators, hospital beds to protect frontliners and attend to those who are sick. This inventory of requirements is critical so groups who want to help can plug in where they are needed.
In previous disasters, the National Disaster Risk Reduction and Management Council (NDRRMC) used to have a National Incident Management System that tracks needs and actions done. This is critical because it prevents bottlenecks in action and information flow, and allows needs to be addressed faster.
The same setup at the national level is then echoed by local disaster management councils at the provincial, city, municipal, and barangay levels. In this setup, citizens and the private sector are not seen as potential victims. Rather they play an active role in helping address the crisis as well.

Step 4: Recover, improve resilience
Lockdowns and quarantines cannot be forever. We need to plan on how and when to get society moving again.
The danger right now with the lockdowns, according to the WHO, is that the disease may jump back up when those movement restrictions and lockdowns are lifted. To prevent this, strong public health measures need to be put in place.
The outbreak and the lockdown will have tremendous socio-political and economic effects. A number of excellent studies on how the Philippines can get back on its feet are worth examining. One worth looking into is a discussion paper written by noted economists from the University of the Philippines School of Economics.
Entitled, “A Philippine Social Protection and Economic Recovery Plan,” its recommendations include measures for social protection, preserving jobs and businesses, providing liquidity, and finally, ensuring transparency and accountability.
One key point that needs to be highlighted is the need for transparency and accountability.
To say that “Congress will exercise its power to check” is not enough. Establishing clear guidelines for distribution of scarce resources is critical. Putting up mechanisms that will help the public track and independently verify where funds went is crucial in building the trust and confidence of all sectors.
Leadership, connecting echo chambers, healing polarization
My final point here has to do with the kind of leadership we need in these trying times.
Managing a complex effort like containing the COVID-19 menace and getting people to work together as a collective so that the country can “heal as one” requires a leader and a manager who is conscious of the science, has experience managing crises, and can traverse the opposing ends of the political spectrum.
For the Philippines to “heal as one,” we need to heal the wounds of polarization that continue to plague this land. Leaders should be humble enough to acknowledge what they do not know and what inputs they need from others.
Make no mistake, if not handled right, this crisis could ruin political careers. Whether or not he deserved it, politicians should remember the experience of Mar Roxas during Yolanda. Hindi ito panahon ng pagpapa-guwapo. (This is not the time for politicians to make themselves look good.)
People are grieving. Trouble is simmering. People are angry, and rightfully so. People are frustrated, and rightfully so.
Leaders need to start listening and acting fast. – Rappler.com
Add a comment
How does this make you feel?
There are no comments yet. Add your comment to start the conversation.