SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.
MANILA, Philippines – In an ideal world, every Filipino would have access to a test, a clinic, and a doctor if they were sick. Feeling a little bit like you could have COVID-19? Reach for that antigen test or head over to a testing site with affordable prices and timely results. Sick with the virus? Go to the nearest primary care provider. In need of more advanced care? You’ll have your doctor, who can manage your treatment and refer you to the right hospital, while recovery won’t burn a hole in your pocket.
In a more realistic world, though, things aren’t so straightforward. Experience symptoms and you’re lucky if you can leave work to get a test, and afford it. Actually sick with COVID-19 and it’ll be a plus if you had a primary care center near your home. In need of professional care, most Filipinos will reflexively make their way to a hospital – where a bed may or may not be available, depending on when you ask. Once it’s time to pay, that’s another challenge altogether.
For anyone who could get COVID-19 or any other disease (and that’s anyone, really), the situation is untenable. And yet, over two years into a pandemic, one of the biggest health crises ever to hit the country, this is what it is like in the Philippines.
More deaths than normal
To grasp the toll of COVID-19 in the Philippines, John Wong, an epidemiologist and co-founder of public health research firm EpiMetrics, prefers to consider excess mortality. The figure tries to account not only for deaths that occurred due to the virus, but also those that took place “either because of COVID or because of our response to COVID.” It also includes deaths that did not occur but would have occurred in more “normal” times, like those due to air pollution.
In tracking excess deaths, we’re able to estimate for these varying deaths to see how many people died in a particular place during a particular period, compared to how many would have died if a particular circumstance, like a pandemic, didn’t occur at all.
Although the official COVID-19 death tally in the Philippines is at nearly 60,500 as of June 20, 2022, the Philippine Statistics Authority reported excess deaths of at least 43,782 from 2020 to 2021. This means nearly 44,000 more Filipinos died on an annual basis in 2020 to 2021 compared to the average annual number of deaths in the previous five years.
That figure would place the country “somewhere in the middle,” according to Wong. Not the best, but not the worst either, among middle-income countries.
But a glimpse of the absolute numbers alone should be enough to invoke pause.
“For public health, it’s the absolute number which is important. The proportion may be small because we’re a big population, but deaths are deaths, right?” Wong said. “[For] every death, there’s a family that survives it.”
While it is now well-known that COVID-19 is deadly, the virus also bore a hidden toll beyond it. People who needed consultation or care for other diseases, but were too afraid to seek care for fear of catching the virus, saw their health worsen. Those who did muster the courage to go to health centers were many times turned away because of limited capacity. There were also those who were sick with COVID-19 and would’ve otherwise had a mild bout of the disease, but unknowingly had a comorbidity that complicated the way the virus behaved in their body.
“I would say all three of them, in some way or another, was related also to how we responded to COVID. It could be inadequate primary care, hospital beds, and critical beds preceding the pandemic. Or it could be the fear generated by the pandemic,” Wong said.
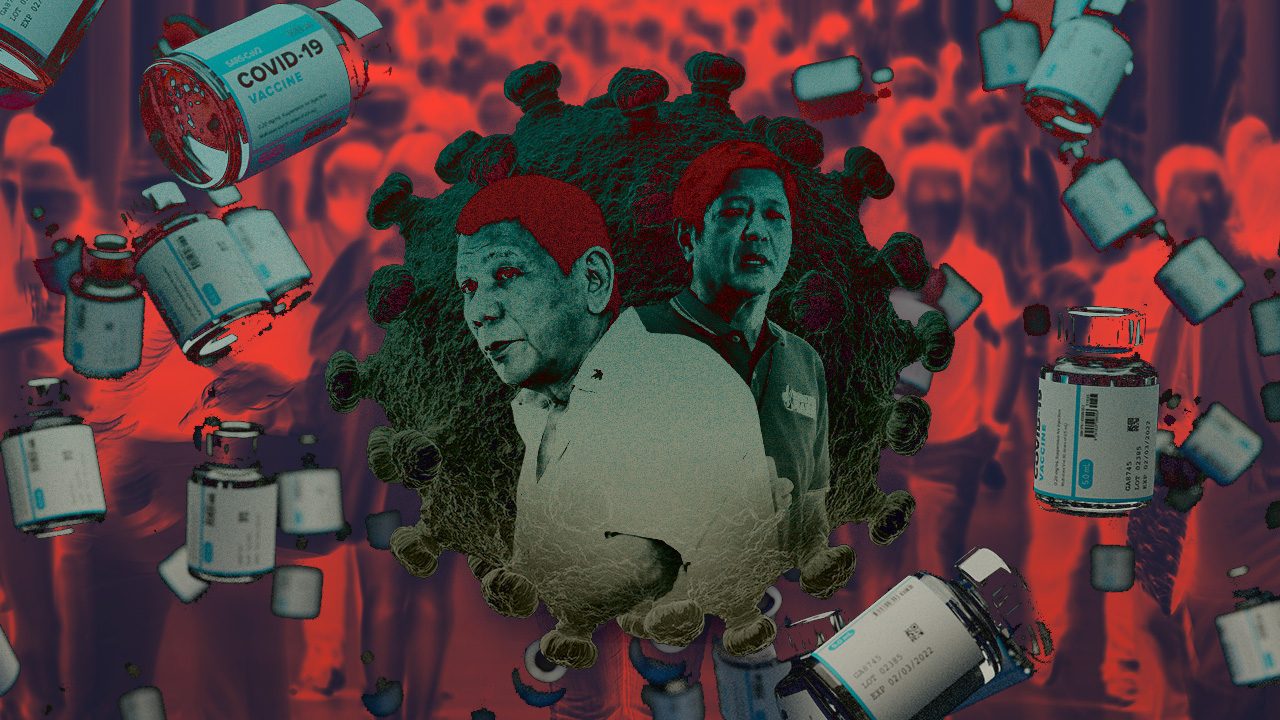
These absolute deaths, then, are reflective of crucial failures seen in the country’s response to COVID-19 and the will to build up its health system to care for all Filipinos. While inequities and vulnerabilities lingered from one administration to the next, the Duterte administration likewise missed an opportunity for change that comes with a life-altering pandemic.
Persistent shortcoming
At every surge the Philippines faced, the shortcomings of the nation’s strategy manifested, and with it inequities persisted. With a new administration set to take office on June 30, how COVID-19 will look like in the country depends on whether these gaps are filled, or ignored.
Experts we spoke to agreed that chief among lapses was the country’s ability to test for the virus. Now, as the country appears to once again be at the start of a new spike in cases driven by more contagious forms of Omicron, just how big a wave we may be in is difficult to determine.
With testing is highly dependent on demand and access – or the lack of it – “for the most part of the pandemic we really haven’t been able to follow the different amount of cases, said Josh San Pedro, a community physician and a co-convenor of the Coalition for People’s Right to Health.

To build capacity then, we’ll need to keep tabs on infections in ways that don’t wholly depend on who can afford and seek out tests. “Are people being tested because they can pay for it? Are people being tested because there is demand for it? Or is there really a fixed amount [of tests] that our surveillance units are doing to ensure that we’re properly monitoring the situation?” San Pedro posed.
Rontgene Solante, an infectious disease specialist at San Lazaro Hospital, agreed: “Part of the healthcare infrastructure is to equip these health facilities with good laboratories so that we don’t need to spend out of our pockets for lab tests. These should be shouldered by the government because we’re in a pandemic.”
Right now, testing to this scale may feel far-fetched. While surveillance systems for other infectious diseases like the flu also existed before the pandemic, the Duterte government was unable to scale them fast enough to handle the deluge in cases.
“For COVID-19, even at the peak for capacity, some provinces still did not have access,” Wong said.
Setting up this capability to test at least at the level of provinces would help not only with COVID-19, but other diseases, too. The Philippines has been able to mount pretty extensive surveillance networks in the past. An example of this would be testing for tuberculosis, which is the country’s most mature health program. RT-PCR testing for the disease can be done at the regional, provincial, city, and, in some cases, even municipal levels.
Granted, tuberculosis programs in the Philippines have existed for nearly a century, but with COVID-19 here forever, it pays to take the long view. Once people are able to test and a better picture of infections is gained, strategies to respond can stay in lock-step with the virus.
Gamble with virus
Coupled with testing is the ability to get treated afterwards, if necessary. Until today, it would be difficult for all Filipinos to receive advanced care if a surge were to occur again or a variant pops up and thwarts the immunity we’ve built.
With expanded primary care under the Universal Health Care (UHC) Law yet to be fully implemented, hospital capacity for both regular and critical care remain limited. As a result, Filipinos had unequal access to necessary care that could mean life or death.
Steps were taken to increase bed capacity over the past two years, but mostly on the regional level. In many provinces, dedicated beds for critical care, for instance, remain lacking.
“Can you imagine you have a critical care patient and then from a certain province you have to rush him all the way to the regional center rather than to the capitol?” Wong said. “There was a lot of money going around during the pandemic, we should have spent some of it building up critical care capacities at least within provincial levels or within city levels.”

According to the Commission on Population and Development, it was during the pandemic that the Philippines saw the largest number of deaths in a single year since World War II. In some cases, people died from conditions that would otherwise been manageable had they gotten treated earlier.
“Even if they weren’t emergency cases to begin with, they become emergency cases because of the lack of access, the lack of continuity or continuous care for these patients,” San Pedro said.
This won’t be a problem just for COVID-19, but other possible pandemics in the future. Until health systems are strengthened to provide people with the care they need from communities up to more advanced care, the country takes a gamble every time cases swell or new, more formidable form of viruses emerge.
‘To those with a lot, give more’
Along with the failure to address inequities and vulnerabilities exposed by the pandemic, the health crisis showed another grave shortcoming: how, oftentimes, people were valued for their productivity above much else.
In the early days of the health crisis, society identified who “essential workers” were, and they were people working in hospitals, supermarkets, deliveries, and other service industries. In other words, people who couldn’t afford to stay home or whose jobs required them to face risks daily. The sector was prioritized early on, but with a push to return to more “regular” times, will they be neglected once more?

“The pandemic hasn’t ended, but now during regular times, suddenly they’re no longer essential. When they ask for pay increases…it is not prioritized,” Wong said. Health workers have likewise called out the government for promised benefits that remain out of reach, two years beyond the start of the crisis.
The same goes with transportation and places of work – workers are asked to return to the office without much being done to improve ventilation or make public spaces any more safe than when COVID-19 first emerged. It’s also true for housing, education, and other social services, where reforms have yet to overtake the virus.
“A lot of these inequities preceded the pandemic but they made low income population more susceptible,” Wong said.
The same outlook was seen in the government’s vaccine rollout, where aside from high risk sectors, significant weight was placed on an area’s “economic risk” in prioritizing vaccine supplies. This has partly resulted in continued gaps in vaccination rates across the country.
“The message has always been: to those who have a lot, give more,” Wong said. “There is a focus on ‘What is your value to us?’ To productivity, rather than who needs it more.”
In many ways, this implicit message has affected public trust in the country’s response to the virus. The past years have shown that controlling a stealthy virus requires as much social cooperation as it does science-based protocols.
Carin Alejandria, a health and disaster anthropologist, spoke of the need for a “partnership” between the government and the public in dealing with the virus long-term. “On the minimum, the state could provide the necessary protection that its’ population needs,” she said.
A ‘better normal’ is still possible
Into our third year living with COVID-19, the virus’s path toward becoming endemic is clear. How we get there, though, is still largely for government and the public to decide. As much as weaknesses of our response dragged on efforts recover, keeping up with the virus has brought to the fore solutions that could offer a “better normal” with COVID-19.
For one, minimum health protocols to curb the coronavirus showed us that small actions could ripple toward more benefits. Wong pointed to data showing a decrease in mortality for tuberculosis, pneumonia, and influenza deaths because of measures like masking. Sepsis and diarrhea declined too as frequent hand washing was promoted, while transport injuries and other respiratory conditions saw drops in numbers with less traffic on roads.
“A lot of diseases we find sometimes, simple interventions could have prevented these deaths…. If this simple behavior can prevent thousands of deaths wouldn’t we want to do it?” Wong said.
The need to navigate the crisis also saw the health department put in place systems to gather insights from experts and study fast-emerging science on the virus. Solante considers it one of the strongest responses to the pandemic.
“Having that expert group, advising the government when it comes to testing, vaccination, with regards to the ability of the drugs and working with the FDA… that helped a lot,” he said. In particular, building a portfolio of vaccines to purchase, Solante added, meant vaccines were always available – although limited – for groups that needed it most, instead of waiting for Western vaccines which performed better, but would arrive much later.
“There was a lot of criticism, like why we were getting Chinese vaccines, and why not Pfizer or Moderna. It was a crucial decision for us because mRNA vaccines arrived late. We were able to save the lives of our vulnerable population and our healthcare workers,” he said.
As Duterte government had been criticized for appointing military men to the top positions of the country’s pandemic inter-agency task force, Solante considered the move to form experts’ groups “gave the direction where the government should be in.” The country now has five groups of experts tasked to guide government actions and its vaccination program.
Aside from this, technical advisers guide the health department for more strategic response. Still, decisions rest with the President.

Another opportunity
If we’re going to have to live with COVID-19 forever, it’s important to know that a better reality than the one we’re currently trodding through is actually possible. In deciding what kind of future with the virus is acceptable, it also pays to think of the quality of life we want.
“Should people be kept in lockdown to keep the infection rate down? Should they be allowed more access to public spaces? Can the government keep on providing subsidies to augment lockdown impacts on household economy? All these questions need be considered,” Alejandria said.
Oddly enough then, finding a way to exit the pandemic won’t mean moving on from COVID-19. It’ll entail constantly monitoring infection levels, ensuring the spaces we live in and pass through have what they need to keep us safe, and building up an arsenal of treatments to fight it.
Health Undersecretary Maria Rosario Vergeire urged the next administration to implement the UHC law “holistically” and to move with the evidence in responding to the virus. This includes the need for the country to have its own center for infectious diseases, to strengthen health sector “in terms of heightened surveillance, established data management, research, and [a] resilient healthcare system.”
“In this pandemic, we saw how science gives as that upper hand for us to continue our policies and intervention. This is also the way we see how UHC law should be implemented moving forward,” Vergeire said in mix of English and Filipino.
All of this needs the political will to make sure that there are enough funds allocated for a robust response to the virus, as well as the agility to intervene when risks associated with the virus start to climb again.

President-elect Ferdinand Marcos Jr. has much to gain if his government is to seriously take up controlling COVID-19. Not only would it provide an opportunity to prove his leadership, it would also quite literally, save lives. It was the pandemic, after all, that pierced President Rodrigo Duterte’s powerful propaganda machine as the health crisis spurred widespread public frustration on social media to a scale unlike other issues that have hounded his administration.
“Transitions are always opportunities to put things on the agenda so with the new administration…. There’s a political window that’s opening, so we should be ready with the solutions for problems that we’re facing,” Wong said.
At no other point in the pandemic have we been so keenly aware of what needs to be done to improve our future with COVID-19. The only thing left to do is to take up recommendations experts have raised time and again. While it is true that recovering from the pandemic – and steeling ourselves for the next one – will be a mammoth task, it’s also true that longer we wait, the steeper the cost to us all. – Rappler.com
Add a comment
How does this make you feel?


![[Time Trowel] Evolution and the sneakiness of COVID](https://www.rappler.com/tachyon/2024/02/tl-evolution-covid.jpg?resize=257%2C257&crop=455px%2C0px%2C1080px%2C1080px)


![[In This Economy] Is the Philippines quietly getting richer?](https://www.rappler.com/tachyon/2024/04/20240426-Philippines-quietly-getting-richer.jpg?resize=257%2C257&crop=194px%2C0px%2C720px%2C720px)





![[The Slingshot] Alden Delvo’s birthday](https://www.rappler.com/tachyon/2024/04/tl-alden-delvo-birthday.jpg?resize=257%2C257&crop=263px%2C0px%2C720px%2C720px)
![[EDITORIAL] Ang low-intensity warfare ni Marcos kung saan attack dog na ang First Lady](https://www.rappler.com/tachyon/2024/04/animated-liza-marcos-sara-duterte-feud-carousel.jpg?resize=257%2C257&crop=294px%2C0px%2C720px%2C720px)
![[Newsstand] Duterte vs Marcos: A rift impossible to bridge, a wound impossible to heal](https://www.rappler.com/tachyon/2024/04/duterte-marcos-rift-apr-20-2024.jpg?resize=257%2C257&crop=278px%2C0px%2C720px%2C720px)

There are no comments yet. Add your comment to start the conversation.